- BUA
broadband ultrasound attenuation
- BMD
bone mineral density
- C-telopeptide
C-terminal telopeptide of type I collagen
- NEAP
net endogenous acid production
Osteoporosis is a skeletal disorder characterised by low bone mass and microarchitectural deterioration of bone tissue, leading to bone fragility and an increased risk of fracture. Optimum bone health is achieved through the contribution of numerous factors such as genetics, health and nutrition. It is common to consider bone health in terms of Ca intake only. Ca is indeed a critical component of the skeleton; however, bone health is much more complex. Whilst the optimum diet for osteoporosis prevention remains unknown, a variety of nutrients are important to the ageing skeleton including protein and micronutrients such as Ca, K and vitamin K(Reference Lanham-New1, Reference Macdonald, New and Fraser2). There is a growing belief that the Western diet may be a risk factor for osteoporosis through excess acid supply. Fruit and vegetable intake may balance the excess acidity by providing K(Reference Lanham-New1, Reference Macdonald, New and Fraser2). As the major determining factor for osteoporosis is an individual's genetic makeup, which cannot be modified, it is important to identify modifiable risk factors that contribute to bone health and use them in prevention messages to the population. Nutrition is a modifiable factor that has the potential to be altered relatively easily and cheaply.
Osteoporosis
Definition
In 1994 the WHO Working Group defined osteoporosis according to measurements of bone mineral density (BMD) using dual-energy X-ray absorptiometry. Thus, osteoporosis is defined as a bone density T-score of ⩽2·5 sd below normal peak values for young adults(Reference Kanis3). These criteria were initially established for the assessment of osteoporosis in Caucasian women.
Epidemiology
Recent epidemiological data estimate that one in two women and one in five men aged >50 years will suffer from an osteoporotic fracture(Reference Holroyd, Cooper and Dennison4). Thus, it is urgent for public health strategies to reduce the predicted increase in osteoporosis within the aging population by undertaking prevention campaigns. A public health strategy for optimising bone health throughout the life cycle is critically important.
Osteoporosis affects an estimated seventy-five million individuals in Europe, USA and Japan. In 2000 there were approximately 9×106 new osteoporotic fractures(Reference Johnell and Kanis5). Recent epidemiological data from the Third National Health and Nutrition Examination Survey indicate that 13–18% of white American women aged ≥50 years have osteoporosis of the hip(Reference Looker, Orwoll and Johnston6). The lifetime risk in the UK for a hip, spine or forearm fracture at the age of 50 years has been estimated to be 53% in women and 21% in men(Reference Van Staa, Dennison and Leufkens7). The projected rise in osteoporotic fracture worldwide clearly demonstrates that the future impact of osteoporosis will be enormous; the worldwide incidence of hip fracture in men is projected to increase by 310% and 240% in women by 2050(Reference Gullberg, Johnell and Kanis8).
In Switzerland between 2000 and 2020 osteoporotic hip, vertebral and forearm fracture are predicted to increase by 33%, 27% and 19% respectively if present prevention and treatment patterns stay unchanged(Reference Schwenkglenks, Lippuner and Häuselmann9). In terms of duration of hospital stay, the annual cost of hospitalisations for osteoporotic fractures is higher than those for myocardial infarction, stroke and breast cancer(Reference Lippuner, Von Overbeck and Perrelet10). In 2000 62 535 hospitalisations for fractures were registered. The direct medical cost of hospitalisations of patients with osteoporosis and/or related fractures was 357×106 Swiss Francs (£15×106), with hip fractures accounting for approximately half these costs(Reference Lippuner, Golder and Greiner11).
Acid–base balance
Disturbances of acid–base balance in the body are classified as either acidosis, indicating an excess of H+ ions (leading to an acid environment; e.g. metabolic, latent or respiratory acidosis), or alkalosis (leading to a reduction in H+ ions and therefore a more alkaline environment). Such disturbances of acid–base balance are relevant to bone health. In vitro studies have shown that there is an induced Ca efflux from bone as a result of metabolic acidosis(Reference Bushinsky and Frick12), which is the only form of acidosis relevant to bone. A moderate increase in alkaline equivalents (90 mmol potassium citrate/d) has been shown to reduce bone resorption, increase bone formation and improve Ca balance in post-menopausal women(Reference Sellmeyer, Schloetter and Sebastian13).
Measuring acid–base status
During the past few decades a number of researchers have used in vitro methods that are inappropriate to specifically determine the acid- or alkaline-producing potential of the diet(Reference Dwyer, Folukes and Evans14). An in vitro measurement of acid:base has been made by using a calculation model(Reference Remer and Manz15, Reference Remer and Manz16). The net acid load is estimated from average intestinal absorption rates of ingested S-containing protein (cysteine and methionine) and additional minerals as well as an anthropometry-based estimate for organic acid excretion:
(Reference Frassetto, Lanham-New and Macdonald17), where PRAL is potential renal acid load and OAest is estimated organic acids, i.e. estimated urinary organic anions, with these two components calculated as follows (we did not include Na and Cl in the PRAL equation because they are usually balanced in the diet):

Determination of acid:base of foods contributing to the overall diet consumed by individuals and population groups is a practical and useful method that can be used in assessing the role of the skeleton in acid–base homeostasis(Reference New18). PRAL has been estimated for a variety of foods items using nutrient data expressed on a per 100 g food basis for protein (methionine, cysteine), P, Cl, K, Mg, Ca and Na (Table 1)(Reference Remer and Manz16).
Table 1. Estimated potential renal acid load (PRAL) in a variety of foods items (from Remer & Manz(Reference Remer and Manz16))
Nutritional factors that influence acid–base balance
Nutrition has long been known to strongly influence acid–base balance in human subjects(Reference Remer19). Intakes of K, Mg and fruit and vegetables have been associated with a more alkaline environment in the human body and therefore have a beneficial effect in relation to bone health(Reference New, Robins and Campbell20).
Indeed, Western diets consumed by adults generate 50–100 mEq acid/d(Reference Vormann and Remer21). Thus, healthy adults consuming such a diet are at risk of chronic low-grade metabolic acidosis, which worsens with age as a result of a decline in kidney function(Reference Frassetto, Curtis Morris and Sebastian22).
Role of the skeleton
Maintenance of acid–base homeostasis is tightly regulated in the extracellular fluid at pH 7·4 ±0·05(Reference New18). Almost every biological process in the human body is dependent on the acid–base balance, including bone metabolism. Bone contributes to acid–base homeostasis as it delivers cations such as Mg, K, Ca and Na, which can be associated with alkali salts such as citrate or carbonate. Over time, an overstimulation of this process will lead to the dissolution of the bone mineral content and hence to a reduction in bone mass(Reference New18, Reference Frassetto, Curtis Morris and Sebastian22). Thus, long-term nutritional acid load may be harmful to bone health.
Protein
Protein is an important macronutrient contributing to BMD. Indeed, sufficient dietary intake appears to have a beneficial effect on bone healing. Supplementation with 20 g protein improves fracture healing and reduces bone loss in elderly subjects; the mechanism appearing to be at least partially through an increase in insulin-like growth factor 1, which stimulates proliferation and differentiation of osteoblasts(Reference Bonjour, Schürch, Chevalley, Ammann and Rizzoli23). However, protein has an acidic effect on bone, which is thought to be undesirable. More precisely, two mechanisms come into play: excess protein induces an increase in renal Ca excretion; the metabolism of the S amino acids (methionine and cysteine) generates an acid load, which results in a reduction in blood and urinary pH(Reference Frassetto, Curtis Morris and Sebastian22, Reference Barzel24, Reference Reid and New25). However, it has been suggested that high-protein diets are associated with an increased risk of fracture when Ca is low, but there is no overall association between total protein and fracture risk with high Ca intake(Reference Dargent-Molina, Sabia and Touvier26). Furthermore, a study of 161 post-menopausal women has suggested that protein intake is positively associated with areal BMD, but benefit at the lumbar spine is offset by a negative impact of the protein S acid load(Reference Thorpe, Mojtahedi and Chapman-Novakofski27). However, it has also been suggested that the negative association between meat intake and BMD may be a reflection of an inadequate consumption of fruit and vegetables rather than an excessive consumption of meat(Reference Heaney and Layman28).
In vitro studies
In vitro studies have shown that metabolic acidosis induces a Ca efflux from bone(Reference Bushinsky and Frick12). It has been demonstrated that the acidification of bone may not be linked only to osteoclastic activity; cultured osteoblasts show reduced collagen synthesis and mineralisation in an acidic environment(Reference Bushinsky29, Reference Frick and Bushinsky30). In both the animal and human model an acid environment is associated with a negative Ca balance and increased bone loss(Reference Lemann, Litzow and Lennon31–Reference Tucker, Hannan and Kiel33). Any reduction in extracellular pH enhances osteoclastic activity(Reference Arnett and Dempster34). Even a small change in pH, approximately (pH 7·1) but not exactly at the physiological level (pH 7·4), stimulates osteoclasts(Reference Arnett and Spowage35). On a long-term nutritional acidic load, pH is kept constant at the expense of bone, which delivers the buffering substances through bone resorption(Reference Green and Kleeman36).
In vivo studies
In vivo studies in healthy subjects have shown that supplements of KHCO3, potassium citrate and even bicarbonate-rich mineral water decrease calciuria and bone resorption markers(Reference Sellmeyer, Schloetter and Sebastian13, Reference Sellmeyer, Schloetter and Sebastian37–Reference Sebastian, Harris and Ottaway39). In healthy male volunteers an acid-forming diet increases urinary Ca excretion by 74% and urinary C-terminal telopeptide of type I collagen (C-telopeptide) excretion by 19% when compared with an alkali (base-forming) diet(Reference Buclin, Cosma and Appenzeller40) (Fig. 1). In cross-sectional studies assessment of the acid:base value has shown that there is a correlation between the nutritional acid load and bone health measured by bone ultrasound(Reference Welch, Bingham and Reeve41) or dual-energy X-ray absorptiometry(Reference New, Macdonald and Campbell42). The Dietary Approaches to Stop Hypertension Trial, which examined the effects of two dietary patterns in 186 adults aged 23–76 years, has compared an experimental Ca-rich diet emphasising fruits, vegetables, whole grains, poultry, fish, nuts and low-fat dairy products with the typical American diet as the control diet. The experimental diet was found to reduce serum osteocalcin by 8–11% and C-telopeptide by 16–18% (P<0·001)(Reference Lin, Gointy and Appel43). However, a recent randomised placebo-controlled study has shown no effect of K supplementation(Reference Macdonald, Black and Aucott44). It was found that potassium citrate supplementation for 2 years does not decrease bone turnover or increase BMD at the spine or hip in post-menopausal healthy women. Moreover, in the group of women who received a supplement of 300 g fruit and vegetables no impact on bone turnover or BMD was observed(Reference Macdonald, Black and Aucott44). Furthermore, the findings of the EVAluation of Nutrients Intakes and Bone Ultra Sound Study (discussed later) have led to the hypothesis that very elderly subjects may be more sensitive to nutritional interventions. In a healthy population other factors such as weight and muscle mass have a substantial effect on bone(Reference Edelstein and Barrett-Connor45, Reference Segal, Torner and Yang46).
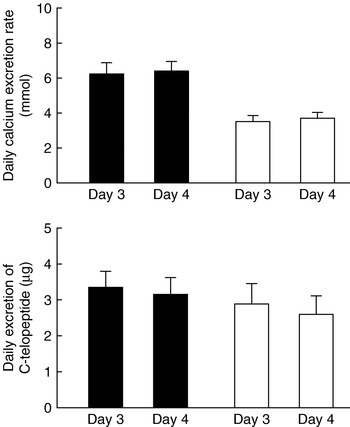
Fig. 1. Mean daily excretion rates of calcium and C-terminal telopeptide of type I collagen (C-telopeptide) for healthy male volunteers (n 8; age 22–31 years) receiving an acid-forming diet (▪) or a base-forming diet (□) with no calcium supplement on day 3 and 1 g calcium supplement on day 4 in a double-cross-over design study. To obtain optimal compliance both diets consisted of alternation of two daily menus, one for days 1 and 3, the other for days 2 and 4. Values are means with their standard errors represented by vertical bars. The effect of diet was significant for calcium (P=0·0002) and C-telopeptide (P=0·01). Calcium supplement had no significant effect. (From Buclin et al.(Reference Buclin, Cosma and Appenzeller40); with kind permission of Springer Science and Business Media.)
Results from the EVAluation of Nutrients Intakes and Bone Ultra Sound Study
Development of a Swiss FFQ
Few studies have been undertaken in very elderly women (>75 years), who are at major risk of osteoporosis risk. As part of the EVAluation of Nutrients Intakes and Bone Ultra Sound Study on osteoporosis in a Swiss very elderly population the influence of dietary intake and acid load on bone health indices was examined in a cohort of 401 ambulatory women (mean age 80·6 years) from the Lausanne area, an urban area of approximately 200 000 inhabitants. A detailed FFQ was developed, cross-validated against a further forty-four 4 d weighed records and the short- (1 month; n 15) and long-term (12 months; n 14) reproducibility examined(Reference Wynn Dumartheray, Krieg and Cornuz47). No significant difference was found between mean energy intakes by 4 d weighed records and the FFQ (6548 (sd 1469) kJ (1565 (sd 351) kcal) and 6867 (sd 2189) kJ (1641 (sd 523) kcal) respectively). Mean crude nutrient intakes were also found to be similar (paired t test), ranging from P=0·13 for K to P=0·48 for Mg. Similar results were found in the reproducibility studies.
Nutrient intake of the EVAluation of Nutrients Intakes and Bone Ultra Sound Study population
The validated FFQ was administered to the cohort of 401 subjects to assess dietary intake(Reference Wynn Dumartheray, Krieg and Cornuz48). The mean daily energy intake was found to be 6460 (sd 1874) kJ (1544 (sd 447·7) kcal), with a protein intake of 65·2 (sd 19·9) g, i.e. 1·03 g/kg body weight per d. The mean daily intakes for energy, fat, carbohydrate, Ca, Mg, vitamin C, D and E were found to be below their respective recommended nutrient intakes(Reference Martin49), while protein, P, K, Fe and vitamin B6 intakes were above their respective recommended nutrient intakes(Reference Martin49) (Table 2). The NEAP for each subject was also calculated using the PRAL equation (Table 2).
Table 2. A comparison of daily dietary intake, as recorded by FFQ, and recommended nutrient intakes (RNI) for 401 very elderly Swiss women (mean age 80·6 years)
NEAP, net endogenous acid production.
* Range.
Thus, the recommendation to optimise dietary intake is energy-dense foods rich in carbohydrate, Mg, Ca, vitamin D and E as well as regular sunshine exposure.
Association between net endogenous acid production estimates and bone ultrasound
The association between NEAP estimates and bone ultrasound results was assessed in the cohort of 401 subjects(Reference Wynn, Lanham-New and Krieg50). No significant effects of the acid load were observed in the whole group, which led to a separate assessment of those women who had a history of fracture (n 256). Fig. 2 shows broadband ultrasound attenuation (BUA) for these 256 women stratified by tertiles of NEAP. Associations were found between higher BUA and both lower estimates of NEAP (r −0·142, P<0·05) and higher estimates of Ca and K (r 0·151 and 0·134 respectively, P<0·05), with the differences remaining significant after adjustment for age, BMI and osteoporosis treatment. The stepwise regression analysis included BUA, NEAP, BMI, osteoporosis treatment, mini nutritional assessment and age. It explains 7·6% of the variation in BUA. BMI and osteoporosis treatment explained 6·3% and NEAP 1·3% of the variation (P<0·05); it is known that ⩽80% of the variance is explained by genetic factors.
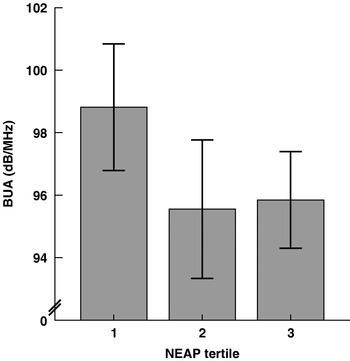
Fig. 2. Broadband ultrasound attenuation (BUA) in the 256 elderly women from the EVAluation of Nutrients Intakes and Bone Ultra Sound Study with fractures stratified by tertiles of net endogenous acid production (NEAP). Values are means and standard deviations represented by vertical bars for eighty-six, seventy-eight and ninety-two subjects for tertiles 1, 2 and 3 respectively. The mean NEAP values for tertiles 1, 2 and 3 were –15·4, –2·6 and 8·3 mEq/d respectively. The mean scores of BUA for the three groups were significantly different: P=0·03 (one-way ANOVA with a post hoc test (Tukey test)); P=0·03 (F test for linearity). Comparison of the means for BUA by tertiles of NEAP (post hoc test (Tukey test)) showed trends: tertile 1 v. tertile 2, P=0·052; tertile 1 v. tertile 3, P=0·07. (From Wynn et al.(Reference Wynn, Lanham-New and Krieg50).)
Thus, the findings suggest that lower estimates of NEAP (i.e. more-alkaline diets) are significantly associated with higher BUA measured by bone ultrasound in the subgroup of elderly women who had a history of fractures. High acid load may be an important additional risk factor that might be particularly relevant in very elderly patients with an already-high fracture risk. The study adds to knowledge by confirming a positive link between dietary alkalinity and bone health indices in the very elderly.
The influence of drinking mineral water on bone health indices
The positive association between low estimates of dietary acid load and bone ultrasound in women >75 years of age with a history of fracture has led to the investigation of the effect of acid load in a younger population by assessing the effect of drinking mineral water on premenopausal women(Reference Wynn, Krieg and Aeschlimann51). The consumption of mineral water may be an easy and cheap way of influencing the acid–base balance.
A comparison was undertaken of the effect of an alkaline (base-forming) mineral water rich in bicarbonate (mg/l; Ca 547, bicarbonate 2172, sulphate 9; PRAL −11·2 mEq/l) with that of an acid (acid-forming) mineral water rich in Ca only (mg/l; Ca 520, bicarbonate 291, sulphate 1160; PRAL +9·2 mEq/l) on bone markers in young women with a normal Ca intake. Thirty female dietitians aged 26·3 (sd 7·3) years were randomised into two groups, with each group following an identical weighed balanced diet (965 mg Ca/d) and drinking 1·5 litres of the assigned mineral water daily. Changes in blood and urine electrolytes, C-telopeptide, urinary pH and bicarbonate and serum parathyroid hormone were measured after 2 and 4 weeks. No difference was found between the groups at baseline and a similar increase in urinary Ca excretion was observed. Urinary pH and bicarbonate excretion were found to increase with the alkaline mineral water, but not with the acid mineral water. Parathyroid hormone (P=0·022; Fig. 3) and serum C-telopeptide (P=0·023; Fig. 4) were shown to decrease with the alkaline mineral water but not with the acid mineral water. Thus, in Ca sufficiency an acid Ca-rich water has no effect on bone resorption, while an alkaline water rich in bicarbonate leads to a decrease in serum parathyroid hormone and serum-C-telopeptide(Reference Wynn, Krieg and Aeschlimann51). By careful choice of mineral water the population could possibly positively influence their bone health.
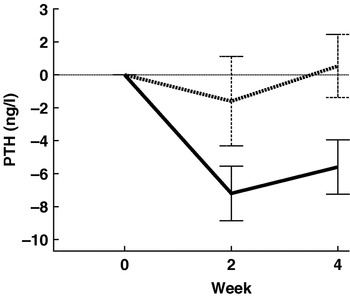
Fig. 3. Mean changes in serum parathyroid hormone (PTH) in premenopausal women (age 26·3 (sd 7·3) years) after 2 and 4 weeks of consuming either an acid-forming mineral water (n 15; ▪ ▪ ▪) or a base-forming mineral water (n 15; ![]() ) and an identical weighed balanced diet (965 mg Ca/d). Values are with their standard errors represented by vertical bars. For the base-forming mineral water the decrease after 4 weeks was significant (P=0·0043). The difference between the two mineral waters at 4 weeks was significant (P=0·022). (Reprinted from Wynn et al.(Reference Wynn, Krieg and Aeschlimann51), with permission from Elsevier.)
) and an identical weighed balanced diet (965 mg Ca/d). Values are with their standard errors represented by vertical bars. For the base-forming mineral water the decrease after 4 weeks was significant (P=0·0043). The difference between the two mineral waters at 4 weeks was significant (P=0·022). (Reprinted from Wynn et al.(Reference Wynn, Krieg and Aeschlimann51), with permission from Elsevier.)
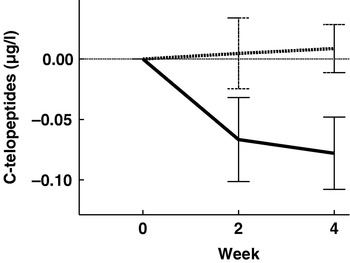
Fig. 4. Mean changes in serum C-terminal telopeptide of type I collagen (C-telopeptides) in premenopausal women (age 26·3 (sd 7·3) years) after 2 and 4 weeks of consuming either an acid-forming mineral water (n 15; ▪ ▪ ▪) or a base-forming mineral water (n 15; ![]() ) and an identical weighed balanced diet (965 mg Ca/d). Values are with their standard errors represented by vertical bars. For the base-forming mineral water the decrease after 4 weeks was significant (P=0·021). The difference between the two mineral waters at 4 weeks was significant (P=0·023). (Reprinted from Wynn et al.(Reference Wynn, Krieg and Aeschlimann51), with permission from Elsevier.)
) and an identical weighed balanced diet (965 mg Ca/d). Values are with their standard errors represented by vertical bars. For the base-forming mineral water the decrease after 4 weeks was significant (P=0·021). The difference between the two mineral waters at 4 weeks was significant (P=0·023). (Reprinted from Wynn et al.(Reference Wynn, Krieg and Aeschlimann51), with permission from Elsevier.)
Concluding remarks
In the present paper the role of acid–base balance and bone health has been discussed. A dietary acid load appears to have a detrimental effect on bone health indices. Long-term studies in post-menopausal women, the group most affected by osteoporosis, would be of major interest to investigate the effect of an acidic diet and whether there is an influence on fracture risk.
Directions for future research work
Future work needs to be undertaken to assess whether certain fruits and vegetables have a more beneficial effect than others. Furthermore, some currently unidentified compounds found in a number of herbs, salad and vegetables have been shown to play a beneficial role in rats(Reference Muhlbauer, Lozano and Reinli52) that is not mediated by their alkalinity but by their pharmacological activity; for example, certain phytonutrients, especially polyphenols, increase osteoblastic activity and decrease osteoclastic activity(Reference Trzeciakiewicz, Habauzit and Horcajada53). A recent study has shown that onion consumption might have a beneficial effect on BMD in peri- and post-menopausal white women aged ≥50 years(Reference Matheson, Arch and Carnemolla54). Thus, increasing the amount of fruit and vegetables in the Western population may be an additional prevention treatment for osteoporosis. However, increasing the daily fruit and vegetable consumption remains a difficult challenge.
It should also be remembered that in man there is a mismatch between the genes and the modern diet that could explain the negative effects of a diet low in K salts on osteoporosis. Man's pre-agricultural hunter–gatherer ancestors consumed wild animal-source foods and uncultivated plant-source foods that would have provided an NaCl-poor K-rich bicarbonate-precursor-rich diet. This K:NaCl has inverted with the dietary shift, as in the modern human diet plant food has fallen and consumption of NaCl has increased(Reference Frassetto, Morris and Sellmeyer55). Human genes are not adapted to this modern diet as the shift to this contemporary diet has occurred too recently for the genome to adjust(Reference Eaton and Cordain56, Reference Eaton, Konner and Shostak57). It has been suggested that the dietary patterns responsible for low-grade metabolic acidosis, as well as low K intakes and high NaCl intakes, contribute to the pathogenesis of osteoporosis and other age-related disorders(Reference Frassetto, Morris and Sellmeyer58, Reference Frassetto, Morris, Sebastian, Burckhardt, Dawson-Hughes and Heaney59).
Acknowledgements
This study was funded by the Foundation for Research on Osteoporosis and Bone Diseases, Lausanne, Switzerland. The authors declare no conflict of interest. E. W. performed the studies and wrote the manuscript, S. A. L-N. provided permanent scientific supervision especially for the nutritional aspects, M. A. K. provided permanent scientific supervision especially for the quantitative ultrasound aspects and P. B. wrote the research protocols, directed and coordinated the studies and supervised the preparation of the manuscript.








