In 2015, the Interventional Working Group of the Association for European Paediatric and Congenital Cardiology (AEPC) published guidelines regarding the training of paediatric cardiologist wishing to further specialise in invasive catheterisation in CHD. Reference Butera, Morgan, Ovaert, Anjos and Spadoni1 As the population of adults with CHD grows and their treatment frequently requires catheter intervention, Reference Aboulhosn, Hijazi and Kavinsky2,Reference Brida, Diller and Nashat3 the guidelines have been extended to include those cardiologists treating this group of patients.
The majority of cardiac catheterisation procedures in CHD are performed with the intention of intervening on specific lesions or problems. Invasive diagnostic procedures are performed less frequently, mainly because current non-invasive options such as echocardiography, MRI, and CT provide very accurate anatomic and functional information. Paediatric and adult cardiologists specialising in invasive catheterisation need to be able to interpret other imaging modalities and have a good working knowledge of the limitations of other imaging modalities in order to adequately plan and carry out procedures. Reference Pushparajah, Duong, Mathur and Babu-Narayan4 Diagnostic catheterisation remains an important tool particularly for direct pressure measurements but also because of the high spatial resolution that angiography offers.
New developments also include catheterisations carried out not only in the classical catheter laboratory or at the bedside but also radiation-free interventions guided by echocardiography or MRI Reference Tzifa, Krombach and Krämer7 Reference Pushparajah, Wong and Bellsham-Revell–9 Basic knowledge about the possibility to perform catheterisation studies without the use of radiation is expected from an advanced trainee.
The collaboration of cardiac surgeons and catheter interventionalists in the catheter laboratory or cardiac theatre in the form of hybrid procedures is a reality, and awareness of the application (and limitations) of the hybrid approach is important for intermediate and advanced trainees. Reference Kalfa and Torres10,Reference Bearl and Fleming11
As in previous versions, Reference Butera, Morgan, Ovaert, Anjos and Spadoni1 all of the recommendations in this document must be considered in the context of local, national, and international regulations, and clinical governance structures and are not intended to override these.
Training in transcatheter intervention in adult CHD
Multi-societal training guidelines relating to transcatheter intervention in adult CHD patients have recently been published. Reference Chessa, Baumgartner and Michel-Behnke12
This document should be viewed as complimenting these training guidelines and can be applied for the training of both paediatric and adult congenital interventionalists. Settings described for paediatrics are applicable for adult congenital programmes, too.
Models of practice and therefore to an extent training reflect differences in local circumstances, and there is no perfect model of interventional care. We would emphasise that opportunities for training and practice in adult CHD interventional practice should not confined to trainees coming from an adult background but are useful for paediatric cardiologists, too. However, it is essential that an adult CHD interventionalist has deep knowledge and experience of congenital cardiac problems, and it is important that interventionalists functioning in this field should do so as part of an expert multidisciplinary team.
Settings
Most cardiac catheterisations for CHD are carried out electively, but acute and emergency procedures occur, mainly in children. It is important that trainees are exposed to procedures in both situations. As indications vary, any cathlab programme undertaking training of paediatric or congenital cardiologists must be within an institution where inpatient and outpatient facilities, intensive care, anaesthesiology, and a cardiac surgical programme for these patients are present. The latter is especially important, as paediatric and congenital cardiac catheterisation, especially interventional procedures, carry risks. Hence, these should be carried out only in departments where congenital cardiac surgery is carried out, too, in case of potential emergencies arising from the catheterisation itself. Reference Krasemann, Berger, Liuba and Thomson13 Lines of communication between the catheterising cardiologist and the cardiac surgeon should be well established and should begin during multidisciplinary meetings for the discussion of procedures. Any trainee involved in catheterisation should also be involved in case planning as well as in early post-catheterisation care. Reference Butera, Morgan, Ovaert, Anjos and Spadoni1,Reference Thomson14,Reference Chessa, Baumgartner and Michel-Behnke15 Although the level of involvement will vary dependent on the level of training, this is important even for beginners.
Regular case reviews and morbidity and mortality meetings should be held to discuss technical, conceptual, and ethical aspects of procedures. Local results should be regularly compared with accepted “standards of care” – usually national audit data or international data published in the literature. The trainee should become more and more involved in all of these aspects. Trained nurses, cardiac physiologists, and radiographers should contribute to procedural planning where appropriate relating to their areas of expertise through consideration of equipment, radiation settings, etc. Their special knowledge will also help the trainee to better understand the complexity of procedures.
The unit lead is responsible for directing the programme and specifically managing the case load, the procedures undertaken in the laboratory as well as offering direction and support for other interventional cardiologists within the team. Reference Butera, Morgan, Ovaert, Anjos and Spadoni1 A named substantive interventional cardiologist should undertake primary responsibility for each trainee or fellow within the programme. This individual should provide support, guidance, and mentorship as well as working with the trainee on paperwork/logbook requirements.
Facilities and equipment
Ideally, a catheterisation laboratory in a training institution should be equipped in accordance with the recommendations of the AEPC, last updated in 2018. As these recommendations were updated recently, we do not include a summary here but refer to the guidelines themselves. Reference Krasemann, Berger, Liuba and Thomson13
Training programme curriculum
Any training programme for paediatric and adult congenital interventionists should include consideration of knowledge, skills, and attitudes. Understanding of the concepts of CHD including natural history and treatment options are a prerequisite for training. In this area, dexterity and the ability to learn and repeat procedures to a high standard are an essential requirement. Finally, ethical considerations need to be taken into account when considering complex interventions in complex patients. Obtaining this overall skill set is a major undertaking which requires dedication, insight, the ability to self-reflect, and the ability to work constructively within a team. In some trainees, manual skills may come easily, but the attitude towards other aspects of care for patients requiring catheterisation such as communication and the acceptance of own shortfalls may not be as well developed. These trainees need special attention and guidance.
Conduct of training
Trainees should be supported to interpret clinical information in context of the patient history, non-invasive findings, and the pre-procedural evaluation and planning of procedures. These should include a consideration of risks, benefits, advantages, and disadvantages of interventional procedure versus alternatives. The trainee should be encouraged to present these data appropriately, for example, during multidisciplinary meetings. Reference Abu-Zidan and Premadasa16
The trainee should discuss her/his preliminary plan of treatment with supervising senior staff and obtain informed consent initially under supervision, but later independently. Adequate documentation, including aims of the intervention, technical considerations, potential risks, and complications is important.
During catheter procedures, the trainee needs to understand the use of radiation and its risks adhering to the “as-low-as-reasonably achievable” (ALARA) principles. Reference Osei, Hayman, Sutton and Pass17,Reference Justino18 Attending a radiation protection course is mandatory ideally before or early in training.
The trainee will initially mainly observe, but then become increasingly involved in cases, starting with patient positioning, equipment preparation, setting up an aseptic scrub table (initially under supervision, i.e., by a qualified cath scrub nurse) and planning of procedures as well as gaining knowledge of the catheter material. In addition, trainees need to learn to assist the primary operator in a reasonable and then anticipatory way. The next step is obtaining skills in vascular access and then subsequently guiding catheters. Interpretation of the obtained catheter data should be assessed regularly by the supervisor.
After the procedure, the trainee with the aid of the trainer needs to critically appraise the procedure and interpret and discuss data obtained.
Post-procedural patient care is an essential part of training. This includes training in and subsequently direct care for a patient after a procedure under general anaesthesia, communicating with anaesthesists, managing the access sites, monitoring for post-procedural complications, ordering and interpretation of post-procedural investigations and discharge planning. Communication with patients and/or parents as well as caregivers should also be done by the trainee, initially under supervision, but over time independently. There should be an opportunity for regular debriefing with the trainer assuming a mentorship role both formally as a route to documenting achievements and milestones in training, but also informally to develop a constructive trainer–trainee relationship.
Training for paediatric and congenital cardiologists in training (basic level)
Interventional congenital catheterisation is usually carried out as part of a programme consisting of paediatric cardiology, general paediatrics, and acute subspecialties, including neonatology and cardiac surgery. Hence, knowledge of these fields is essential to understand and discuss indications and results of these procedures with these subspecialties. The guidelines of the AEPC regarding training including all these domains are updated regularly. 19 For adult congenital heart programmes carrying out catheterisations, understanding of the patients history and interventions (both surgical and in the catheter laboratory) in the past is essential.
Carrying out cardiac catheterisations as first operator at this level of training is not mandatory.
During core training in Paediatric Cardiology, trainees should at the relevant time in training be exposed, under supervision, to cardiac catheterisation (see training recommendations for Paediatric Cardiology from the AEPC on the AEPC website. 19 ). Each trainee should be exposed to 50 catheterisations, including the pre- and post-procedural care and the interpretation of the obtained catheter data and how it relates to other investigations.
A basic level of training for paediatric and adult congenital interventions should provide the trainee with introductory knowledge of haemodynamics, angiography, radiation safety, indications, risks, limitations, and benefits of catheter procedures in patients with CHD. This includes knowledge of the use of ionising radiation and the ALARA principle. Reference Osei, Hayman, Sutton and Pass17,Reference Justino18 Ideally, the trainee should also be involved in emergency procedures like balloon atrial septostomies and pericardiocentesis. If direct opportunities are limited, then a thorough understanding of emergency procedures-indications, techniques, and complications should be obtained.
A summary of the required knowledge, skills, and attitudes is shown in Table 1.
Table 1. Knowledge, skills, and attitude at different levels of training.

Training for paediatric and congenital cardiologists specialising in catheterisation techniques (intermediate and advanced level)
After successfully completing training at a basic level, including adequate assessments of competence the trainee, in conjunction a trainer may decide to move to training at the next level.
Intermediate level
At intermediate level, a trainee congenital cardiologist specialising in catheterisation should plan and in some cases perform diagnostic cardiac catheterisation as first operator, including single-ventricle evaluation and selected pulmonary hypertension studies. The trainee should work towards performing 100 interventional procedures, of which approximately 50 should be (at least in part) as first operator, under supervision. Direct participation in any part of a catheter study counts towards total numbers.
Usually, to achieve the number of procedures, this level of training will require at least 12 months.
Increasing depth of knowledge in the planning of procedures and interpretation of the acquired data is expected, and the trainee should be responsible for the presentation of catheter information during multidisciplinary meetings.
A summary of the required knowledge, skills, and attitudes is shown in Table 1.
Advanced level
This level of training requires at least 12 months in a dedicated fellow position. Training is summative and at advanced level, the trainee should look to build on knowledge and skills learned in the intermediate stage. In addition to more “simple” interventions and diagnostic catheterisations, the trainee should actively plan and take part in more complex interventions eventually progressing to the point that they can take the lead in selected cases. Eventually, the trainee should demonstrate the skills required to perform these complex cases as the main operator, although still under support by an experienced substative interventionalist. Progress needs to be monitored and documented regularly.
Integration of different imaging modalities during catheterisation procedures, that is, transoesophageal echocardiography, image overlay from previously acquired cross-sectional imaging like MRI or CT, including strengths and weaknesses should be recognised and understood by the trainee. Reference Pushparajah, Duong, Mathur and Babu-Narayan4 Reference Kang, Armstrong, Krings and Benson–6 The potential role of rotational angiography in certain clinical situations should be considered. Reference Tzifa, Krombach and Krämer7 Trainees need to know about the use of additional advanced imaging but also about the limitations of the different techniques applied.
Since around 15 years, MRI-guided interventions have been performed. Reference Tzifa, Krombach and Krämer7 MRI-guided catheterisation of both diagnostic and interventional allow catheterisation without the use of radiation. Reference Veeram Reddy, Arar and Zahr8,Reference Pushparajah, Wong and Bellsham-Revell9 The trainee should be aware of the possibility to perform radiation-free cardiac catheterisation studies. However, this must be put within the local context and the local availability of such facilities.
Depending on institutional practice, the trainee should be involved in hybrid procedures from the planning stage to procedural execution.
To achieve an adequate level, it is possible that the trainee may need to spent time in a larger institution where a (near) full-time focus on catheterisation is a reasonable prospect and advanced techniques are regularly in use. At this level of training, the trainee should perform at least 150 catheter interventions on the top of intermediate training level as first operator. A higher number of procedures is desirable and will contribute to developing the trainees skills to further depth.
An advanced trainee should have exposure to intervention in patients of all ages and in order to achieve this special provision may need to be made, for example, time within an adult CHD lab for a paediatric cardiologist based in a children’s hospital, and in a paediatric cath lab for an adult congenital interventional trainee.
Experience at this level should include angioplasty and stenting of aortic coarctation and branch pulmonary arteries, embolisation and retrieval techniques, and ideally percutaneous valve insertion and VSD closure. Consideration of potential complications related to catheterisation, use of stents or devices, need to be discussed in advance with more senior colleagues, and bail-out plans should be made by the trainee.
A summary of the required knowledge, skills, and attitudes is shown in Table 1.
At any level of training, simulation training, the use of augmented reality, and also training on decision making can be important for the progress of the trainee.
Assessment
As already stated, training is summative and progress will be different for each individual. It is important to assess the trainee regularly to document progress, identify deficiencies, and plan further training needs. Ideally, regular formative and summative assessments should be performed and form part of documentation of training in line with local and national regulations and practices.
Mandatory courses (radiation protection and morphology) should be documented, as well as any other courses or conferences relevant to the field of catheter interventions the trainee attended. The content should be reflected on during assessment meetings.
Comprehensive logbook
The trainee should keep a comprehensive logbook of all activities related to cardiac catheterisation as outlined in Table 1. At each level of training, the logbook will be a central piece of evidence of training. The logbook should contain a list of all procedures carried out and that should include technical details, complications and their management, and personal reflections. During regular training meetings, the logbook will form an important tool for discussion of achievements and needs between the trainer and trainee. It is essential that not only technicalities are discussed during training meetings but also the time for reflection is given.
In addition, regular direct observation of skills should be carried out in a structured way to allow the trainee to self-reflect on comments received. Reference Bindal, Goodyear, Bindal and Wall20 Also, the trainee should receive advice and recommendations on how to improve skills. An example of a form for such structured assessment is shown in Figure 1 (which has not changed since the last recommendations were published in 2015).
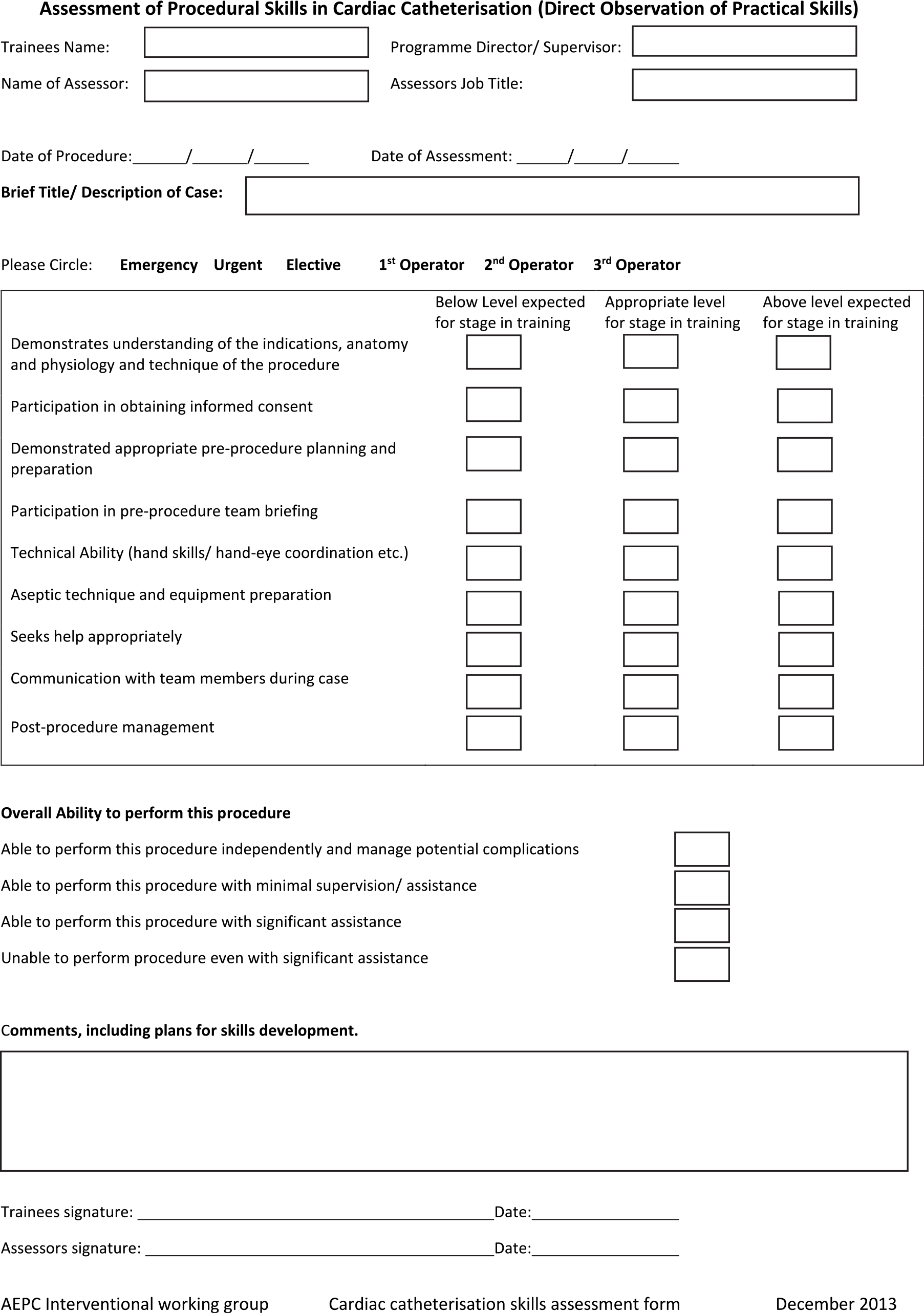
Figure 1. Direct observation of practical skills form for use to assess procedural planning and skills in the congenital cardiac catheterisation laboratory.
An example of a structured procedure log is shown in Table 2.
Table 2. Example of logbook.

Whilst feedback from the trainer is important for the trainee regarding the three domains of knowledge, skills, and attitude, these can also be assessed formally by other team members, that is, by a multi-source feedback. This allows an assessment not only on the specific skills and knowledge necessary in the catheterisation laboratory itself but also on attitude and performance within the broader team. Reference Stevens, Read, Baines, Chatterjee and Archer21,Reference St John, Tong, Li and Wilbur22 In most instances, these will be carried out in the form of anonymised structured questionnaires which can be distributed, collected, and collated before feeding back the results to the trainee. Reference Stevens, Read, Baines, Chatterjee and Archer21
For every level of the training, a documented personal development plan based on the requirements as described above is useful and provides a framework for a discussion of achievements and expectations. Short-term and medium-term goals should be written down, signed by both the trainer and the trainee, and be used at appraisal meetings to evaluate the progress of the trainee against these previously agreed aims. Such appraisal meetings should be held at least annually. These yearly reviews may also be useful for local statutory and academic training bodies.
The trainee in difficulty
Documentation of assessment is important, especially if previously agreed goals have not been reached. Shortcomings and weaknesses should be identified, and potential solutions or remedies for the trainee must then be agreed. In the unfortunate situation where the trainee repeatedly fails to meet objectives, despite adequate support and guidance the trainee may be deemed unsuitable to become an independently working congenital interventionalist. To reach this conclusion, it is essential that deficiencies in knowledge, skills, or an attitude incompatible with teamworking/high-quality patient care should be accurately documented and discussed with the trainee. A trainee in this situation will require discussion within the wider local medical training infrastructure (e.g., the overarching training “Deanery”) where formal advice and support for both the trainee and the training programme can and should be obtained.
Where it is clear that a trainee will not progress within the interventional field but has attributes that are compatible with substantive practice in congenital cardiology adequate support should be given in developing other career options within the specialty.
Conclusions
Training in interventional congenital cardiology is complex because it requires not only manual skills and dexterity but also a thorough knowledge of pathology and haemodynamics across a great variety of patients, and of materials and devices. To obtain adequate exposure requires extensive training which may be long and arduous.
Also, once a trainee successfully reaches advanced level of training, he/she can get a role as junior interventionalist in a team. Learning never stops, and mentoring may be ongoing even after the training has formally been finished. Working in teams will allow any interventionalist to develop further independent of his/her level of experience.
The responsibility of the trainers cannot be overestimated. Leading by example and in a constructive manner is hugely important for a trainees development. Ultimately, training should provide opportunities for the trainee to grow into the role of an interventionalist who, at the end of the training, can confidently consider indications, carry out standard procedures safely and independently, and appraise himself and the institutional approaches critically, thus contributing to the development of the specialty in a collaborative manner. In many cases, this will require a trainee to need to move between units and even countries to seek and obtain the experience required. The success of mentorship has been shown for cardiac surgery and in the catheterisation laboratory. Reference Nassour, Balentine and Boland23–Reference Bagai, O’Brien and Al Lawati25
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1047951123000823.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Competing interest
None.






