Introduction
Mid-aortic syndrome is a rare vascular disease characterised by narrowing of lower thoracic and upper abdominal aorta with or without involvement of renal arteries, causing severe hypertension and heart failure. Reference Rumman, Nickel and Matsuda-Abedini1,Reference Forman, Sinskey and Shalabi2 The main aetiology of mid-aortic syndrome is idiopathic, followed by other congenital or acquired disorders. Reference Lazea, Al-Khzouz and Sufana3 Most patients are diagnosed in childhood and young adult, typically under 18 years of age Reference Musajee, Gasparini, Stewart, Karunanithy, Sinha and Sallam4 , with mid-aortic syndrome being sporadically diagnosed in neonates and infants. Reference Zhao, Zhu and Zhao5,Reference Izraelit, Kim, Ratner, Levasseur, Seigle and Krishnamurthy6 We present an unusual case of mid-aortic syndrome with secondary dilated cardiomyopathy in a 2-month-old female who showed spontaneous normalisation of the abdominal aorta over time during anti-heart failure treatment.
Case report
A 2-month-old female with newly confirmed dilated left ventricle due to symptoms of respiratory distress and cough was transferred to our paediatric ICU for further treatment. Echocardiography on admission showed that her left ventricle was dilated up to 33.3 mm (Z-score: 5.62) at end-diastole (Figure 1A), and left ventricle ejection fraction was measured at 10% despite continuous administration of inotropic agents including dopamine (5 mcg/kg/min) and dobutamine (5 mcg/kg/min). Initial laboratory studies indicated a serum lactate level of 2.5 mmol/L (normal range: 0.5–1), which was mildly increased. Serum B-type natriuretic peptide was 288 pg/mL (normal range: 0–100). Fortunately, both her renal and liver functions were found to be normal. To improve the symptoms and signs related to aggravating heart failure, we added oral digoxin (5 mcg/kg/dose every 12 hours) and diuretics (furosemide: 1 mg/kg/day, spironolactone: 1 mg/kg/day), and angiotensin converting enzyme inhibitor (captopril 0.3 mg/kg/dose every 8 hours). In addition, due to a gradual increase in blood pressure approaching hypertensive levels during this treatment regimen, oral beta-blocker (carvedilol 0.04 mg/kg/dose every 12 hours) was started concurrently on the 2nd day of admission. Despite her decreased cardiac contractility, she frequently exhibited uncontrolled elevated blood pressure, reaching up to 125/72 mmHg [95th percentile cut-off for infants aged 2 months: 100/67 mmHg] over time, measured non-invasively in the left arm using a cuff. On the 6th under administration of anti-hypertensive agents, blood pressure measurements in four extremities were as follows; right arm 91/49 mmHg, left arm 93/58 mmHg, right leg 87/48 mmHg, and left leg 87/46 mmHg. For the differential diagnosis for persistent hypertension in the upper extremities, CT angiography of aorta was performed, which showed a diffusely small calibre of the abdominal aorta and its branches with no evidence of coarctation of the proximal descending thoracic aorta (Figure 1B and 1C). Laboratory test revealed hyperreninemic hyperaldosteronism (renin activity > 80 ng/mL/hr [normal range: 0.3–2.9] and aldosterone 205.0 ng/dL [normal range: 3–16]). Under the diagnosis of secondary hypertension possibly resulting from idiopathic mid-aortic syndrome, considering the CT images of the aorta and the laboratory test results, we continued to prescribe captopril and carvedilol for anti-heart failure and anti-hypertensive treatment. During a hospitalisation period about one and a half months, her heart failure symptoms (such as chest retraction, tachypnoea, and tachycardia) improved even after tapering-off the inotropic agents. Her left ventricle end-diastolic dimension decreased to 30.2 mm (Z-score: 4.15) and left ventricle ejection fraction improved up to 33.1% on the last echocardiography before discharge. Thus, she was discharged from the hospital on the 46th hospital day with following anti-heart failure medications: digoxin 5 mcg/kg/dose every 12 hours, furosemide 0.6 mg/kg/dose every 12 hours, spironolactone 0.6 mg/kg/dose every 12 hours, captopril 0.5 mg/kg/dose every 8 hours, and carvedilol 0.25 mg/kg/dose every 12 hours. During admission, genetic testing revealed a novel unclassified variant of TMPO gene, c.1316A > T (p. Glu439Val), whose role remains unclear yet. At 2 years of age, we decided to discontinue digoxin, furosemide, and spironolactone when her cardiac function was assessed as almost normal (left ventricle ejection fraction: 51.6%). Eight years after diagnosis, a follow-up CT angiography of the aorta showed an interval increase in the diameter of the abdominal aorta and slightly small-sized renal arteries with no focal stenosis (Figure 2A and 2B). Interestingly, there seemed to be a spontaneous resolution of her mid-aortic syndrome without any endovascular or surgical intervention. Additionally, her blood pressure profile was normal between the upper (99/55 mmHg) and lower extremities (108/54 mmHg) considering her age of 8 years. At the latest outpatient clinic, 9 years after diagnosis, she had no symptoms, and her left ventricle end-diastolic dimension was 40.1 mm (Z-score: 1.08) with an left ventricle ejection fraction of 56.5% (Figure 2C) on low-dose enalapril (0.06 mg/kg/dose once daily) only.
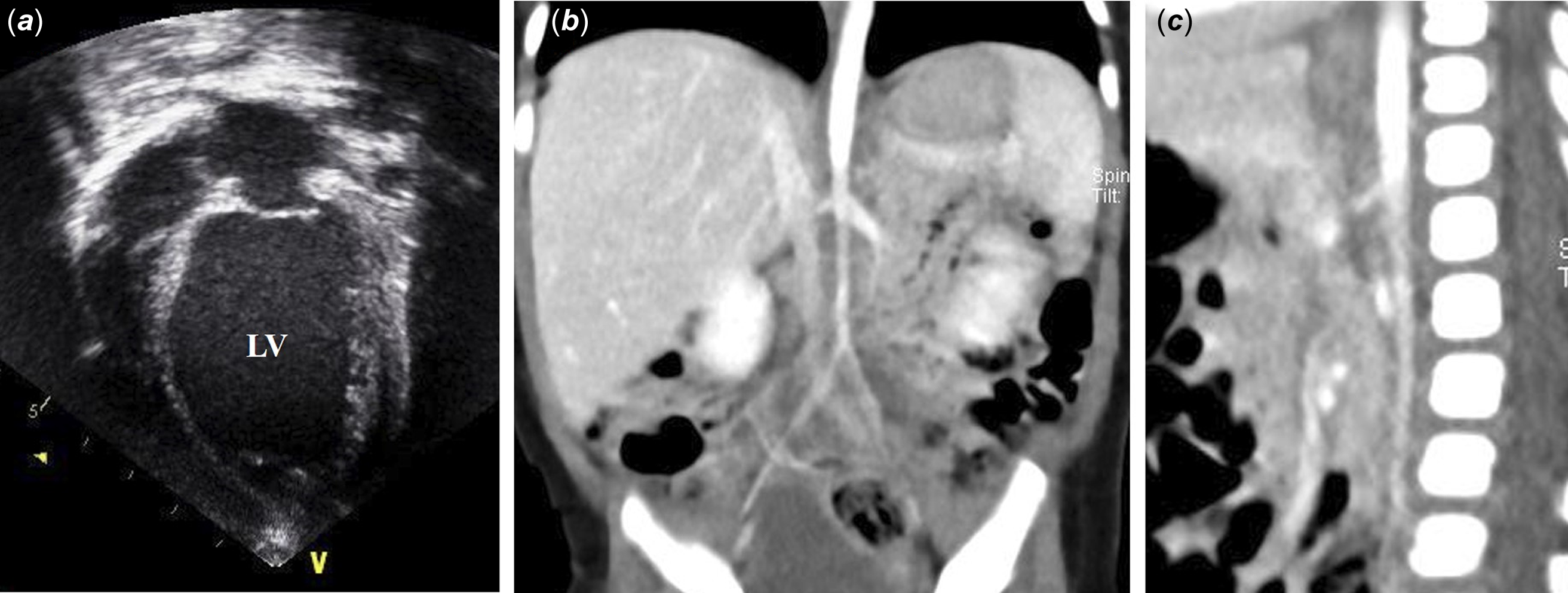
Figure 1. ( a ) Initial transthoracic echocardiography. Echocardiography revealed a dilated LV with diameter up to 33.3 mm (Z-score: 5.62) at end-diastole and LV EF of 10% at the time of diagnosis. ( b and c ) Initial CT angiogram of aorta. There were diffuse hypoplasia of the lower abdominal aorta and its branches, as well as small size of both renal arteries. LV = left ventricle, EF = ejection fraction.
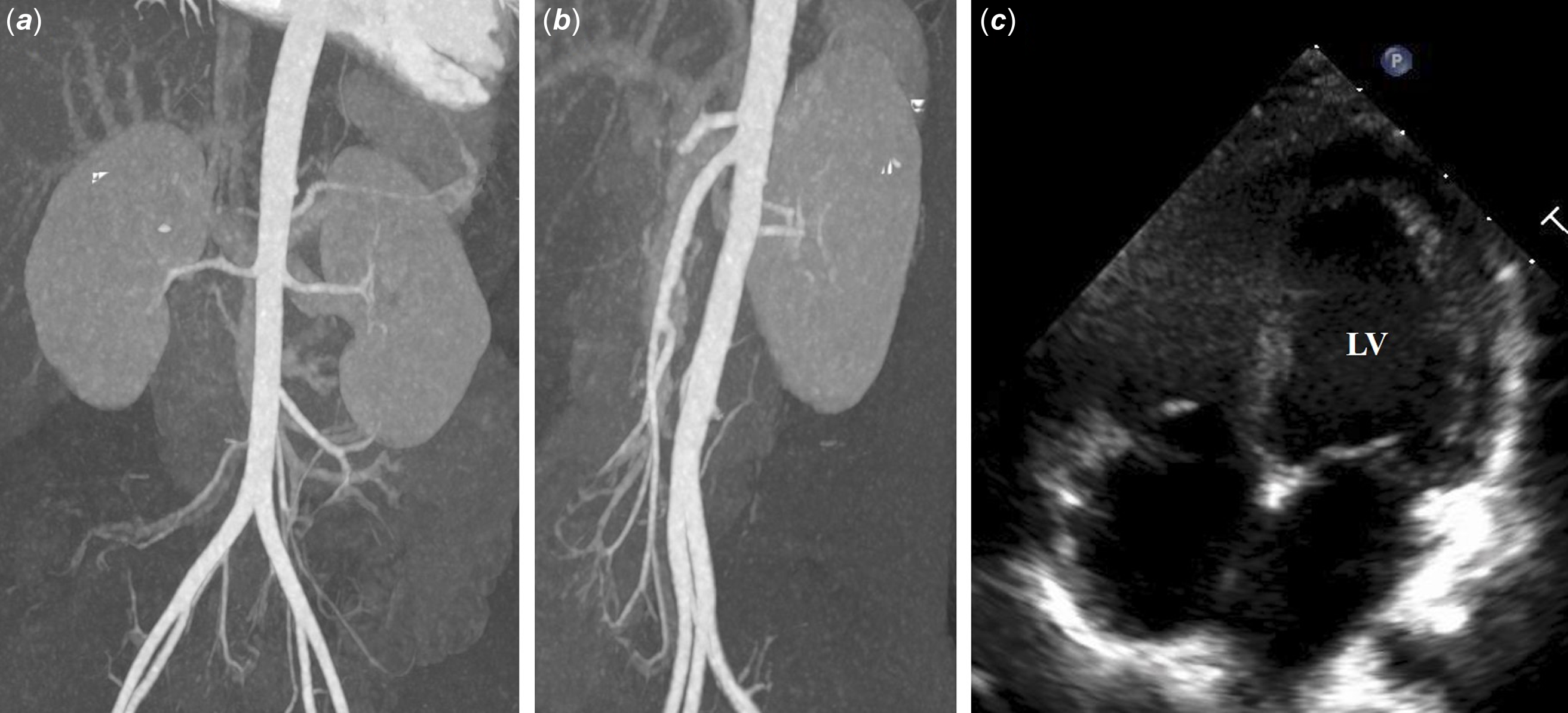
Figure 2. ( a and b ) Follow-up CT angiogram of the aorta 8 years after initial diagnosis. The patient had an interval increase and normalisation in the diameter of the abdominal aorta (proximal abdominal aorta: 10.5 mm, aorta at the level of renal arteries: 8.2 mm) and slightly small-sized both renal arteries (right: 2.3 mm, left: 2.6 mm) without focal stenosis. ( c ) Latest transthoracic echocardiography 9 years after initial diagnosis. Echocardiography showed a regressed LV with diameter up to 40.1 mm (Z-score: 1.08) at end-diastole and normalised LV EF of 56.5%. LV = left ventricle, EF = ejection fraction.
Discussion
Mid-aortic syndrome is an uncommon vascular disorder characterised by stenosis of the lower thoracic or abdominal aorta. Despite its low incidence, poor prognosis and high mortality have been reported in infantile mid-aortic syndrome with refractory hypertension. Reference Rumman, Nickel and Matsuda-Abedini1,Reference Forman, Sinskey and Shalabi2 Mid-aortic syndrome-related diseases may include genetic disorders such as neurofibromatosis-1, Williams syndrome, and Alagille syndrome, as well as inflammatory disorders like Takayasu’s arteritis, which can cause arterial stenosis. Nonetheless, the aetiology of idiopathic mid-aortic syndrome remains largely unknown. Reference Lazea, Al-Khzouz and Sufana3 Mid-aortic syndrome is usually diagnosed by CT angiography or MR angiography, which shows diffuse or segmental stenosis of the abdominal aorta. Reference Hirsch and Hong7 Additional classification can be made based on location and severity of aortic stenosis in aorta and its major arterial branches. Reference Musajee, Gasparini, Stewart, Karunanithy, Sinha and Sallam4,Reference Delis and Gloviczki8 In general, medical therapy, endovascular procedures, and surgical options are considered for the treatment of mid-aortic syndrome. Establishing a standard of management protocol for mid-aortic syndrome patients is challenging due to the rarity of the disease and the limited available evidence. However, it is evident that patients with poorly controlled blood pressure or worsening heart failure, despite appropriate medical therapy, benefit from invasive managements, including endovascular intervention and open surgical repair. Reference Forman, Sinskey and Shalabi2,Reference Delis and Gloviczki8,Reference Chalmers, Dhadwal, Deal, Sever and Wolfe9 Most reported cases of infantile mid-aortic syndrome involved with severe aortic stenosis that required interventional treatment. Reference Zhao, Zhu and Zhao5,Reference Thompson, Sprouse, Mir and Burkhart10 Additionally, idiopathic mid-aortic syndrome often leads to refractory hypertension necessitating invasive options. Reference Rumman, Nickel and Matsuda-Abedini1,Reference Musajee, Gasparini, Stewart, Karunanithy, Sinha and Sallam4 However, in neonatal or infant patients, endovascular or surgical intervention can be demanding due to the lack of consensus on indications for invasive approaches, the small size of the vessels, the high risk of operative or anaesthetic complications, or inoperability. According to a recent review by Rumman et al., 14.4% of patients became normotensive, and 35.8% showed improvement with conservative medical treatment. Reference Rumman, Nickel and Matsuda-Abedini1 Given the sufficient outcome of medical treatment in cases with mild-to-moderate stenosis, appropriate medical management can be important and beneficial, especially for neonates or infants. In our case, a 2-month-old patient was initially diagnosed with heart failure associated with dilated cardiomyopathy. When investigating her birth history, she was born at 40 weeks and 5 days of gestation with a birth weight of 3.56 kg via caesarean section. In other words, there were no notable perinatal conditions aside from the caesarean delivery, and she had no significant medical issues until her first visit to our hospital. There is no history of any intra-arterial catheterisation, particularly umbilical arterial lines. She presented with cough and respiratory distress as her primary manifestations but did not initially exhibit definite hypertension. After admission to our paediatric ICU, she also experienced intermittent oliguria requiring proper diuretic supports and apparent hypertensive blood pressure in the upper extremities, despite decreased cardiac function, which provided clues for a diagnosis of mid-aortic syndrome. Although the blood pressure difference in her four extremities appeared mild, our prior experience with another patient who had mid-aortic syndrome and exhibited a similar blood pressure discrepancy led us to perform CT angiography for her whole abdomen to rule out mid-aortic syndrome aggressively. During the course of her treatment, the patient did not show other well-known causes of mid-aortic syndrome, such as the previously mentioned congenital or acquired disorders, nor did the CT imaging show evidence of external compression from any adjacent mass-like lesion. Therefore, we suspected that the most likely cause of mid-aortic syndrome in this patient was idiopathic. Thankfully, in our patient, a trial of medical management as the first-line approach for hypertension and heart failure was sufficient. Moreover, there was a radiologically confirmed spontaneous relief of her mid-aortic syndrome without any invasive intervention during follow-up. Our case emphasises the rare disease course of mid-aortic syndrome in infancy, presenting cardiomyopathy and heart failure. Despite the young diagnostic age and idiopathic cause, the significant narrowing of the abdominal aorta showed interval regression while our patient received consistent medical treatment. This indicates effective management of the systemic effects caused by mid-aortic syndrome through medication, allowing the patient to achieve stable conditions supportive of sufficient growth and natural recovery. Consequently, this resulted in the spontaneous normalisation of the abdominal aortic narrowing.
Financial support
None.
Competing interests
None.
Ethical standard
Not applicable.





