A number of research studies indicate that people exposed to major natural disasters are at increased risk for a variety of mental health problems. For instance, a study of Thai survivors of the 2004 Indian Ocean tsunami found elevated rates of post-traumatic stress disorder (PTSD), anxiety, and depression 8 weeks and 9 months post-tsunami.Reference van Griensven, Chakkraband, Thienkrua, Pengjuntr, Cardozo and Tantipiwatanaskul 1 However, most of such research has focused on the mental health functioning of populations exposed to a major catastrophic disaster,Reference Karamustafalioglu, Zohar, Guveli, Gal, Bakim and Fostick 2 – Reference Tang 4 but relatively little is known about the mental health functioning of populations exposed to less severe but more frequent disasters, such as the recurrent flooding of the Mekong Delta in Southeast Asia. Theoretically, exposure to more frequent but less severe disasters could result in increased psychological resiliency, with such populations functioning relatively well despite exposure to natural disasters.Reference Almedom 5 (For the purpose of this paper, we refer to destructive natural events, including storms, floods, landslides, etc. as ‘natural disasters’, recognising that they may range from destructive but not catastrophic to truly catastrophic). Such exposure could provide opportunities to develop in a non-overwhelming context both psychological and environmental coping skills to overcome disaster-related adversity.Reference Almedom 5 , Reference Cordova, Cunningham, Carlson and Andrykowski 6 Supporting such a position Pooley and colleagues found a positive relation between disaster-related stress and ‘disaster growth’ (i.e. the ability to develop strength from exposure to natural disasters) among people living in cyclone-prone areas of northwest Australia.Reference Pooley, Cohen, O'Connor and Taylor 7 On the other hand, it is possible that repeated exposure to even non-severe natural disasters may increase risk for mental health problems, as people's coping abilities are exceeded and drained. Supporting this position, a study of flood victims in the United Kingdom found that previous exposure to flooding was a risk factor rather than a protective factor for increased psychological distress after a flood.Reference Mason, Andrews and Upton 8
People living in low- and middle-income countries (LMIC) are at increased risk of physical injury, death, communicable diseases, etc., in the event of a natural disaster.Reference Kahn 9 During 1970–2008, over 95% of deaths from natural disasters occurred in LMIC.Reference Field, Barros, Stocker, Qin, Dokken and Ebi 10 This is partially due to the fact that the effects of natural events in LMIC are compounded by poor quality of building construction, a lack of disaster response infrastructure, easily disrupted jobs, etc., resulting in a greater likelihood that any particular natural event will reach the level of a natural ‘disaster’. In LMIC, those most frequently exposed to disasters also tend to be the more vulnerable members of the community (i.e. more likely to have low income and resources).Reference Kim 11 Chronic stress related to poverty and occupational insecurity may compound the effects of a specific disaster, placing people at greater risk for subsequent mental health problems. The study of the mental health and functioning of populations exposed to frequent natural disasters becomes particularly critical in the face of global climate change. Recent estimates project rising sea-levels, more frequent and severe flooding, and more intense tropical cyclones.Reference Field, Barros, Stocker, Qin, Dokken and Ebi 10 , 12 The low-quality infrastructure, restricted water resources and reliance on fragile crop production or fishing industries, etc., associated with LMIC status place people living in LMIC at greatest risk from such effects of climate change. 12 – Reference Confalonieri, Menne, Akhtar, Ebi, Hauengue, Kovats, Parry, Canziani, Palutikof, Van der Linden and Hanson 15
The present study focuses on Vietnam which, although recently moved from low-income to lower-middle-income economic status, still has 43.4% of its population at or below the $2/day poverty level due to substantial income inequity. 16 The country suffers from large disparities in healthcare provision as well.Reference Vuong, Van Ginneken, Morris, Ha and Busse 17 In Vietnam, even lower-level storms such as tropical depressions can result in significant death rates and destruction. For example, tropical depression 06W in 2007 resulted in severe flooding that caused over 60 deaths in Vietnam. 18 More generally, Vietnam is among the five countries in the world most vulnerable to climate change, and natural disasters are estimated to currently reduce Vietnam's GDP by about 1.5%. 12 The purpose of the present study was to assess the mental health and life functioning and their predictors among residents of central coastal Vietnam, an area characterised by (a) high risk for repeated natural disasters, occurring (b) in the LMIC context of chronic poverty and other related risk factors. The second primary purpose was to determine the extent to which exposure to frequent typhoons and other major storms and related factors were associated with impaired health and life functioning. Standard mental health measures for depression (PHQ-9), anxiety (GAD-7), traumatic stress (PDS), somatic syndrome (SCL-90-R), alcohol dependence (ICD-10 criteria adapted for Vietnam), self-perceived physical health status (SF-36 general physical health item) and functional impairment (life functioning section of the PDS) were used to assess mental health, self-perceived physical health and life functioning, with caseness determined using each measure's algorithm. Predictors evaluated included demographic characteristics, financial stress, past exposure to major storms and past exposure to traumatic events (including traumatic storm exposure).
Method
Setting
The present study focused on coastal central Vietnam, a largely rural region with a history of typhoons, floods, landsides and other natural disasters. 19 – Reference Thomas, Christiaensen, Do and Trung 22 From 2003 to 2012, eight typhoons, seven tropical storms and seven tropical depressions impacted this broad area. 23 People living in coastal central Vietnam are generally poor with low education levels. The median annual family income (which typically represents income from several adults) in this region is $1244 (compared with the national per capita GNI of $1550), with less than 40% of adults completing high school.Reference Weiss, Dang, Trung, Nguyen, Thuy and Pollack 24
Study population
The purpose of the sampling frame was to obtain a representative sample of adults (individuals 18 years or older) living in areas of central coastal Vietnam frequently exposed to typhoons, tropical storms and flooding. Five provinces covering the middle approximate 210 km of coastline of central Vietnam were chosen. Within each province, two coastal village districts (an administrative unit of approximately 10 000 people) were selected from geographically separate areas, for a total of ten data collection sites. Within each village district, 100 adults were randomly selected for participation from public population lists. In Vietnam, all citizens must register with neighbourhood authorities. These population lists are public record and include basic demographic information. As often is the case in Vietnam, the participation rate was very high, likely due to citizens’ general tendency to participate in activities that are seen as useful for the good of society.Reference Weiss, Dang, Trung, Nguyen, Thuy and Pollack 24 , Reference McKelvey, Davies, Sang, Pickering and Tu 25 A total of 1000 potential participants were initially selected for recruitment, and of these 10 declined to participate or were unable to be contacted. These potential participants were replaced with another community member matched on age (within 5 years), gender and occupation. Interviews took place between May 2013 and July 2013. The final sample consisted of 1000 adults, with 80% (804) of the sample providing valid data on all measures and 99% (999) providing valid data on one or more measures after final data review. Participants ranged from 18 to 85 years of age with a median age of 42 years (Table 1).
Table 1 Demographic and background characteristics, by province
| Binh Dinh (n=200) | Da Nang (n=200) | Hue (n=200) | Quang Nam (n=200) | Quang Ngai (n=200) | Total (n=1000) | |
|---|---|---|---|---|---|---|
| Age, years: median (range) | 44 (21–67) | 38 (20–69) | 38 (20–68) | 46 (21–85) | 44 (18–82) | 42 (18–85) |
| Female, n (%) | 122 (61%) | 109 (55%) | 98 (49%) | 122 (61%) | 112 (56%) | 563 (56%) |
| Marital status, n (%) | ||||||
| Single | 7 (4%) | 34 (17%) | 26 (13%) | 14 (7%) | 17 (9%) | 98 (10%) |
| Married | 175 (91%) | 148 (74%) | 158 (81%) | 166 (85%) | 147 (82%) | 794 (83%) |
| Divorced/separated | 2 (1%) | 7 (4%) | 6 (3%) | 0 (0%) | 3 (2%) | 18 (2%) |
| Widowed | 8 (4%) | 10 (5%) | 5 (3%) | 16 (8%) | 13 (7%) | 52 (5%) |
| Education, years: median (range) | 9 (0–12) | 10 (0–12) | 6 (0–16) | 8 (0–16) | 7 (0–12) | 8 (0–16) |
| Occupation, n (%) | ||||||
| Market seller | 35 (22%) | 25 (19%) | 10 (6%) | 5 (3%) | 16 (10%) | 91 (11%) |
| Farmer | 32 (20%) | 7 (5%) | 57 (33%) | 137 (78%) | 90 (56%) | 323 (40%) |
| Fisherman | 3 (2%) | 3 (2%) | 79 (46%) | 0 (0%) | 15 (9%) | 100 (13%) |
| Labourer/factory worker | 42 (27%) | 64 (48%) | 3 (2%) | 8 (5%) | 14 (9%) | 131 (16%) |
| Office worker | 5 (3%) | 11 (8%) | 4 (2%) | 10 (6%) | 5 (3%) | 35 (4%) |
| Homemaker | 32 (20%) | 14 (10%) | 17 (10%) | 3 (2%) | 18 (11%) | 84 (11%) |
| Retired | 8 (5%) | 10 (7%) | 2 (1%) | 12 (7%) | 3 (2%) | 35 (4%) |
| Employment status, n (%) | ||||||
| Stable | 111 (56%) | 120 (60%) | 148 (76%) | 166 (86%) | 97 (56%) | 642 (67%) |
| Not stable | 46 (23%) | 48 (24%) | 32 (16%) | 17 (9%) | 57 (33%) | 200 (21%) |
| Unemployed | 40 (20%) | 32 (16%) | 14 (7%) | 10 (5%) | 18 (10%) | 114 (12%) |
| Financial stress, n (%) | ||||||
| Low | 135 (68%) | 148 (74%) | 164 (82%) | 157 (79%) | 77 (43%) | 681 (70%) |
| Moderate | 45 (23%) | 44 (22%) | 34 (17%) | 40 (20%) | 85 (47%) | 248 (25%) |
| High | 19 (10%) | 7 (4%) | 2 (1%) | 3 (2%) | 18 (10%) | 49 (5%) |
| Major storms, n (%) | ||||||
| 0 | 0 (0%) | 1 (1%) | 4 (2%) | 0 (0%) | 0 (0%) | 5 (1%) |
| 1 | 8 (4%) | 17 (9%) | 57 (29%) | 105 (53%) | 43 (23%) | 230 (23%) |
| 2 | 26 (13%) | 60 (30%) | 63 (32%) | 33 (17%) | 35 (19%) | 217 (22%) |
| 3 | 48 (24%) | 46 (23%) | 19 (10%) | 13 (7%) | 26 (14%) | 152 (15%) |
| 4 or more | 118 (59%) | 73 (37%) | 55 (28%) | 48 (24%) | 85 (45%) | 379 (39%) |
| Traumatic major storm exposure, n (%) | ||||||
| No | 55 (28%) | 67 (34%) | 43 (25%) | 24 (12%) | 29 (15%) | 218 (23%) |
| Yes | 145 (73%) | 131 (66%) | 129 (75%) | 176 (88%) | 161 (85%) | 742 (77%) |
| Number of traumatic events, a n (%) | ||||||
| 0 | 24 (12%) | 49 (25%) | 34 (17%) | 20 (10%) | 14 (7%) | 141 (14%) |
| 1 | 105 (53%) | 97 (49%) | 73 (37%) | 141 (71%) | 83 (44%) | 499 (50%) |
| 2 | 58 (29%) | 42 (21%) | 77 (39%) | 27 (14%) | 58 (31%) | 262 (26%) |
| 3 or more | 13 (7%) | 12 (6%) | 16 (8%) | 12 (6%) | 35 (18%) | 88 (9%) |
a Number of traumatic events includes traumatic major storms.
Procedures
The project was conducted through the Da Nang Psychiatric Hospital (DNPH), the leading psychiatric hospital in central Vietnam, with the support of the provincial psychiatric hospitals in the four other provinces. Human subjects’ approval was obtained from the Da Nang Psychiatric Hospital U.S. FWA IRB (#00011251). Provincial psychiatric hospitals obtained support from the local Community Health Stations (CHS) in participating communities. CHS staff accompanied the data collector to participants’ homes, briefly introduced the project to potential participants, and left. The project data collector described the project in more detail, obtained informed consent from those interested in participating and scheduled a time for the interview. Interviews lasted 1.5–2 h, and participants were given the option of breaking the assessment into two shorter periods. Participants were paid the equivalent of US $7.10 for the interview. Data collectors included physicians, nurses and psychologists who received 5 days of training including: (a) an overview of the study, design and assessment measures; (b) the interview protocol and procedures; (c) how to support participants who might become distressed during the interview. Data collectors received ongoing supervision from the provincial hospital directors.
Mental health was assessed using standard measures including: (1) Patient Health Questionnaire (PHQ-9, assessing depression; internal consistency α=0.87 in current sample),Reference Kroenke, Spitzer and Williams 26 (2) Generalized Anxiety Disorder-7 (GAD-7, α=0.90; GAD symptoms),Reference Spitzer, Kroenke, Williams and Löwe 27 (3) Post-traumatic Diagnostic Scale (PDS, α=0.88; PTSD symptoms),Reference Foa, Cashman, Jaycox and Perry 28 (4) Somatization Scale from the Symptom Checklist-90-R (SCL-90-R, α=0.84); somatic syndrome),Reference Derogatis 29 and (5) alcohol dependence (using a measure developed for this project based on ICD-10 criteria for alcohol dependence syndrome, α=0.80). Overall self-perceived health status was assessed using the (6) Short Form Health Survey (SF-36) general physical health itemReference McHorney, Ware, Lu and Sherbourne 30 and (7) functional impairment was assessed using the life functioning section of the PDS to assess the extent to which over the past month the various mental health symptoms interfered with participants’ life functioning (α=0.94).Reference Foa, Cashman, Jaycox and Perry 28 Caseness for the various measures was determined using each measure's specific algorithm. For measures with multiple levels of caseness (i.e. mild, moderate and severe), the moderate and above cut-off (i.e. moderate or severe) were used in order to identify significant levels of mental health problems.
Past experiences with typhoons and similar major storms were evaluated using the PDS, assessing beliefs during the event (in this case, the major storm) regarding fearing for life of self or other, serious physical injury to self or other (including death to another person) and feeling helpless or feeling terrified. Exposure to other potentially traumatic events (natural disasters other than a major storm; physical or sexual abuse; traffic or industrial accidents; war-related trauma; being imprisoned; ‘other’ including being attacked by a wild animal, near drowning, etc.) was assessed with the same PDS items, for these events. The Chronic Financial Stress measure, which was adapted from similar measures,Reference Butterworth, Rodgers and Windsor 31 , Reference Wrosch, Heckhausen and Lachman 32 contains six items rated on a 1–4 scale that assesses concern related to financial problems (e.g. having insufficient money to obtain needed food) that the family has experienced over the past 6 months. It produces three levels of financial stress (low, moderate, high) based on the cut-offs from the measures from which it was derived.Reference Butterworth, Rodgers and Windsor 31 , Reference Wrosch, Heckhausen and Lachman 32
A US clinical psychologist fluent in Vietnamese and a Vietnamese psychiatrist and Vietnamese clinical psychologist fluent in English applied standard procedures for translating assessment measures for which there was not a pre-existing Vietnamese version.Reference van Widenfelt, Treffers, de Beurs, Siebelink and Koudijs 33 The validity of the translation was checked through independent back-translations. Measures were then reviewed by teams from the five participating provincial psychiatric hospitals for appropriateness for Vietnamese participants, with translations adjusted based on their feedback, and measures re-evaluated, etc.
Statistical analysis
Generalised linear models via Proc Glimmix (SAS 9.4) were used for analyses of risk factors. In these analyses, risk factors were treated as categorical data as listed in Table 3, with binary health and functioning outcomes. The logit link function was used. To control for clustering, Province was included in all inferential risk factor analyses as a random factor. Missing values were treated as missing and excluded from analyses.
To assess the overall relations between the risk factors and health outcomes (as opposed to bivariate relations) we used canonical correlation analysis.Reference Tinsley and Brown 34 Canonical correlation assesses relations between two sets of variables (in this case the [1] risk factors, and [2] the mental health and self-perceived physical health outcomes), estimating weights so as to produce maximal correlation between the resulting pairs of linear composites (canonical variates). As in exploratory factor analysis, (a) canonical variates are extracted in order of the amount of variance explained, with each successive pair of variates (i.e. each dimension) orthogonal to its predecessor, and (b) canonical variates are interpreted by the magnitude of the relation between the latent canonical variate and the observed variables (i.e. the loadings). Thus, a canonical variate is similar to a latent factor in exploratory or confirmatory factor analysis. A loading cut-off of 0.40 was used.Reference Tinsley and Brown 34 Proc Cancorr (SAS 9.4) was used for the canonical correlation analysis, with the covariance matrix externally estimated via Proc Corr for pairwise deletion of missing data. To avoid loss of information associated with dichotomisation, the full scales rather than caseness were analysed.
Role of the funding source
Funding for this study was provided by the US National Institutes of Health (D43-TW009089) and the Royal Norwegian Embassy in Hanoi. The sponsors of the study had no role in study design, data collection, data analysis, data interpretation or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
One thousand individuals were assessed, with 56% (n=563) female, a median age of 42, a median of 8 years’ formal education, and 83% (n=794) married (Table 1); 30% (n=297) of the sample reported moderate to high levels of financial stress, and 33% (n=314) reported not having stable employment or being unemployed. Almost all people in the sample (99%, n=978) had lived through at least 1 typhoon or other major storm in their lifetime, with the median lifetime number of major storms experienced equal to three, and 77% (n=742) of the sample having experienced a traumatic typhoon or other major storm (they had feared for their life or the life of someone close to them etc.) (Table 1). In contrast, approximately 3% of the sample reported lifetime exposure to a traumatic traffic or industrial accident (e.g. with threat of severe injury or death; witnessing someone else die), 2% had experienced a traumatic life-threatening illness, and 3% had experienced an ‘other’ event (e.g. near drowning). For all other categories (e.g. war-related trauma), exposure was less than 1%.
Mental health status and life functioning
Overall, 7% (n=65) of people reported either very good or excellent self-perceived physical health whereas 38% (n=370) reported less than good (fair or poor) health. The caseness rate for current (a) depression was 2% (n=21), (b) GAD 5% (n=45), (c) PTSD 10% (n=97) and (d) somatic syndrome 16% (n=147). Alcohol use was common with 87% (n=367) of males and 18% (n=97) of females reporting that they sometimes drank alcohol; 4% (n=18) of males and no females reported symptoms of alcohol dependence. Overall, 23% (n=227) of the sample met caseness criteria for one or more of these mental health domains, and 22% (n=221) of the total sample reported that their mental health symptoms had a moderate-to-severe impact on their life functioning (Table 2).
Table 2 Current (past month) physical health, mental health and functional impairment, by province
| Binh Dinh, n (%) a (n=200) | Da Nang, n (%) (n=200) | Hue, n (%) (n=200) | Quang Nam, n (%) (n=200) | Quang Ngai, n (%) (n=200) | Total, n (%) (n=1000) | |
|---|---|---|---|---|---|---|
| Physical health b | ||||||
| Poor | 1 (1%) | 19 (10%) | 4 (2%) | 23 (12%) | 24 (13%) | 71 (7%) |
| Fair | 44 (22%) | 61 (31%) | 34 (17%) | 69 (35%) | 91 (51%) | 299 (31%) |
| Good | 129 (65%) | 112 (56%) | 154 (77%) | 89 (45%) | 58 (32%) | 542 (55%) |
| Very good | 24 (12%) | 7 (4%) | 8 (4%) | 18 (9%) | 5 (3%) | 62 (6%) |
| Excellent | 0 (0%) | 1 (1%) | 0 (0%) | 1 (1%) | 1 (1%) | 3 (0%) |
| Depression c | ||||||
| None | 191 (97%) | 170 (92%) | 196 (98%) | 180 (93%) | 149 (87%) | 886 (94%) |
| Mild | 5 (3%) | 11 (6%) | 3 (2%) | 9 (5%) | 11 (6%) | 39 (4%) |
| Moderate | 1 (1%) | 1 (1%) | 0 (0%) | 4 (2%) | 8 (5%) | 14 (1%) |
| Severe | 0 (0%) | 2 (1%) | 1 (1%) | 0 (0%) | 4 (2%) | 7 (1%) |
| Anxiety d | ||||||
| None | 177 (89%) | 156 (78%) | 175 (88%) | 187 (94%) | 130 (72%) | 825 (84%) |
| Mild | 19 (10%) | 30 (15%) | 18 (9%) | 7 (4%) | 35 (19%) | 109 (11%) |
| Moderate | 3 (2%) | 12 (6%) | 5 (3%) | 6 (3%) | 12 (7%) | 38 (4%) |
| Severe | 0 (0%) | 2 (1%) | 2 (1%) | 0 (0%) | 3 (2%) | 7 (1%) |
| PTSD e | 10 (5%) | 18 (9%) | 20 (10%) | 13 (7%) | 36 (20%) | 97 (10%) |
| Somatic syndrome f | ||||||
| None | 189 (95%) | 167 (84%) | 162 (91%) | 100 (62%) | 63 (40%) | 681 (76%) |
| Mild | 7 (4%) | 14 (7%) | 7 (4%) | 16 (10%) | 24 (15%) | 68 (8%) |
| Moderate | 4 (2%) | 14 (7%) | 2 (1%) | 29 (18%) | 36 (23%) | 85 (9%) |
| Severe | 0 (0%) | 5 (3%) | 7 (4%) | 16 (10%) | 34 (22%) | 62 (7%) |
| Alcohol dependence g | 4 (2%) | 7 (4%) | 2 (1%) | 5 (3%) | 0 (0%) | 18 (2%) |
| Any psychiatric disorder | ||||||
| 0 | 184 (92%) | 158 (79%) | 168 (84%) | 144 (72%) | 99 (55%) | 753 (77%) |
| 1 | 12 (6%) | 30 (15%) | 26 (13%) | 42 (21%) | 45 (25%) | 155 (16%) |
| 2 or more | 4 (2%) | 12 (6%) | 6 (3%) | 14 (7%) | 36 (20%) | 72 (7%) |
| Functional impairment h | ||||||
| None | 161 (81%) | 116 (58%) | 161 (81%) | 152 (76%) | 129 (65%) | 719 (72%) |
| Mild | 7 (4%) | 18 (9%) | 9 (5%) | 17 (9%) | 9 (5%) | 60 (6%) |
| Moderate | 27 (14%) | 53 (27%) | 27 (14%) | 19 (10%) | 46 (23%) | 172 (17%) |
| Severe | 5 (3%) | 13 (7%) | 3 (2%) | 12 (6%) | 16 (8%) | 49 (5%) |
a Results presented are based on responses for each cell.
b Self-perceived physical health measured by SF-36 general health item.
c Depression measured by PHQ-9.
d Anxiety measured by GAD-7.
e PTSD measured by PDS.
f Somatic syndrome measured by Somatization Scale from the SCL-90-R.
g Alcohol dependence based on ICD-10 criteria.
h Functional impairment measured by life functioning section of the PDS.
Table 3 Risk for current (past month) physical health, mental health and functional impairment caseness, by risk factor
| Physical health problems a , b n (%) g | Depression b , c n (%) g | Anxiety b , d n (%) g | PTSD b n (%) g | Somatic syndrome b , e n (%) g | Alcohol dependent b n (%) g | Any psychiatric disorder b n (%) g | Comorbid diagnoses b n (%) g | Functional impair-ment b , f n (%) g | |
|---|---|---|---|---|---|---|---|---|---|
| Gender, n (%) | |||||||||
| Female | 255 (46%) A | 12 (2%) | 32 (6%) A | 65 (12%) A | 66 (13%) | 0 (0%) A | 132 (24%) | 40 (7%) | 140 (25%) A |
| Male | 108 (25%) B | 5 (1%) | 10 (2%) B | 27 (6%) B | 40 (11%) | 17 (4%) B | 78 (18%) | 19 (4%) | 73 (17%) B |
| χ2 | 38.78**** | 1.63 | 6.70** | 8.38** | 0.88 | 7.56** | 3.83 | 3.67 | 9.81** |
| Age, years: n (%) | |||||||||
| 17 to 25 | 17 (18%) A | 0 (0%) A | 1 (1%) A | 1 (1%) A | 3 (4%) A | 2 (2%) | 7 (7%) A | 1 (1%) A | 12 (13%) A |
| 26 to 40 | 72 (22%) A | 1 (0%) A | 8 (2%) A | 19 (6%) B | 26 (9%) A | 3 (1%) | 48 (15%) B | 10 (3%) A | 47 (13%) A |
| 41 to 55 | 156 (42%) B | 9 (3%) A | 25 (7%) B | 41 (11%) C | 48 (14%) B | 9 (2%) | 97 (26%) C | 29 (8%) B | 83 (22%) B |
| 56 to 70 | 91 (64%) C | 3 (2%) A | 5 (3%) AB | 21 (15%) C | 21 (16%) B | 4 (3%) | 42 (30%) C | 12 (9%) B | 50 (35%) C |
| 71 to 87 | 32 (88%) D | 7 (21%) B | 2 (7%) AB | 12 (33%) D | 9 (25%) B | 1 (1%) | 19 (52%) D | 8 (23%) C | 22 (60%) D |
| χ2 | 93.60**** | 29.51**** | 11.32* | 31.33**** | 18.35** | 2.83 | 43.52**** | 27.84**** | 51.86**** |
| Education | |||||||||
| None | 99 (69%) A | 10 (7%) A | 12 (8%) A | 28 (19%) A | 27 (19%) A | 2 (1%) | 54 (37%) A | 20 (14%) A | 59 (41%) A |
| Elementary school | 145 (41%) B | 5 (1%) B | 18 (5%) A | 46 (13%) A | 45 (14%) AB | 4 (1%) | 89 (25%) B | 29 (8%) B | 78 (21%) B |
| Middle school | 79 (29%) C | 4 (2%) B | 11 (4%) A | 12 (5%) B | 21 (9%) BC | 6 (2%) | 43 (16%) C | 8 (3%) C | 43 (16%) B |
| High school + | 38 (18%) D | 0 (0%) B | 2 (1%) B | 7 (3%) B | 13 (7%) C | 5 (3%) | 25 (12%) C | 2 (1%) C | 32 (16%) B |
| χ2 | 73.73**** | 16.16** | 11.01* | 31.98**** | 13.43** | 1.82 | 32.88**** | 26.09**** | 32.55**** |
| Marital status | |||||||||
| Not married | 54 (32%) | 5 (3%) | 6 (4%) | 22 (13%) | 16 (10%) | 1 (1%) | 38 (23%) | 10 (6%) | 36 (21%) |
| Married | 299 (38%) | 12 (2%) | 36 (5%) | 70 (9%) | 88 (12%) | 16 (2%) | 170 (21%) | 48 (6%) | 174 (22%) |
| χ2 | 1.58 | 1.50 | 0.38 | 3.24 | 0.43 | 1.70 | 0.12 | 0.01 | 0.04 |
| Employment status | |||||||||
| Stable | 196 (31%) A | 5 (1%) A | 23 (4%) | 40 (6%) A | 54 (9%) A | 12 (2%) | 116 (18%) A | 23 (4%) A | 114 (18%) A |
| Unstable | 94 (47%) B | 6 (3%) B | 14 (7%) | 34 (17%) B | 33 (17%) B | 4 (2%) | 62 (31%) B | 24 (12%) B | 64 (32%) B |
| Unemployed | 65 (57%) B | 5 (5%) B | 4 (3%) | 15 (13%) B | 17 (16%) AB | 1 (1%) | 27 (24%) A , B | 11 (9%) B | 30 (26%) B |
| χ2 | 32.15**** | 9.36** | 4.86 | 20.97**** | 9.35** | 0.77 | 13.15** | 21.09**** | 18.35**** |
| Occupation | |||||||||
| Market seller | 40 (44%) A | 0 (0%) | 3 (3%) | 3 (4%) A | 6 (7%) | 0 (0%) | 11 (12%) A , B | 2 (2%) | 11 (12%) A |
| Farmer | 139 (43%) A | 7 (2%) | 27 (8%) | 51 (16%) A | 47 (17%) | 6 (2%) | 101 (31%) C | 31 (10%) | 101 (31%) B |
| Fisherman | 37 (38%) A | 3 (3%) | 4 (4%) | 9 (9%) A | 7 (8%) | 3 (3%) | 20 (20%) A,B,C | 6 (6%) | 20 (20%) AB |
| Labourer/ factory worker | 27 (21%) B | 2 (1%) | 4 (3%) | 6 (4%) A | 10 (8%) | 6 (5%) | 21 (16%) A , B | 3 (3%) | 21 (16%) A |
| Office worker | 4 (11%) B | 0 (0%) | 0 (0%) | 1 (3%) A | 2 (7%) | 0 (0%) | 3 (7%) A | 1 (2%) | 5 (14%) A |
| Homemaker | 46 (39%) A | 2 (3%) | 4 (5%) | 6 (8%) A | 7 (9%) | 1 (1%) | 11 (14%) A , B | 5 (6%) | 17 (20%) A , B |
| Retired | 52 (18%) A | 0 (0%) | 1 (3%) | 5 (15%) A | 6 (18%) | 0 (0%) | 9 (26%) BC | 3 (10%) | 7 (21%) A , B |
| χ2 | 31.81**** | 2.30 | 7.58 | 18.53** h | 10.92 | 5.70 | 23.82*** | 11.60 | 17.56** |
| Financial stress | |||||||||
| Low | 211 (31%) A | 4 (1%) A | 12 (2%) A | 41 (6%) A | 47 (7%) A | 10 (2%) | 99 (15%) A | 22 (3%) A | 94 (14%) A |
| Moderate | 122 (49%) B | 7 (3%) B | 19 (8%) B | 35 (14%) B | 42 (19%) B | 7 (3%) | 82 (33%) B | 23 (9%) B | 94 (38%) B |
| High | 28 (57%) B | 9 (19%) C | 11 (22%) C | 14 (28%) C | 16 (32%) B | 2 (3%) | 27 (55%) C | 13 (26%) C | 25 (51%) B |
| χ2 | 28.67**** | 35.19**** | 34.88**** | 27.94**** | 32.16**** | 1.71 | 54.19**** | 34.81**** | 71.94**** |
| Number of major storms i | |||||||||
| 1 | 92 (41%) | 3 (1%) | 4 (2%) | 16 (7%) | 19 (10%) | 4 (2%) | 39 (17%) | 8 (4%) | 41 (18%) |
| 2 | 69 (33%) | 3 (2%) | 10 (5%) | 18 (9%) | 21 (11%) | 5 (2%) | 41 (20%) | 12 (6%) | 38 (18%) |
| 3 | 49 (32%) | 2 (2%) | 6 (4%) | 16 (11%) | 20 (14%) | 1 (1%) | 33 (22%) | 9 (6%) | 32 (21%) |
| 4 or more | 145 (39%) | 10 (3%) | 22 (6%) | 40 (11%) | 46 (13%) | 8 (2%) | 92 (25%) | 26 (7%) | 96 (25%) |
| χ2 | 4.50 | 2.15 | 5.05 | 2.71 | 2.54 | 1.28 | 4.61 | 3.27 | 6.65 |
| Traumatic major storm exposure | |||||||||
| No | 52 (25%) A | 2 (1%) | 5 (2%) | 10 (5%) A | 22 (11%) | 5 (3%) | 35 (16%) | 8 (4%) | 31 (14%) A |
| Yes | 299 (41%) B | 14 (2%) | 36 (5%) | 79 (11%) B | 82 (12%) | 12 (2%) | 169 (23%) | 48 (7%) | 177 (24%) B |
| χ2 | 16.28**** | 0.82 | 2.49 | 6.41* | 0.19 | 0.95 | 3.83 | 2.33 | 9.59** |
| Number of traumatic events j | |||||||||
| 0 | 29 (21%) A | 1 (0%) A | 0 (0%) A | 2 (2%) A | 15 (12%) | 2 (1%) | 16 (12%) A | 2 (1%) A | 18 (13%) A |
| 1 | 173 (35%) B | 5 (1%) A | 17 (3%) A | 38 (8%) B | 44 (10%) | 8 (2%) | 93 (19%) A | 21 (4%) A | 87 (17%) A |
| 2 | 105 (41%) B | 9 (4%) A | 18 (7%) B | 35 (14%) C | 30 (13%) | 5 (2%) | 67 (26%) B | 24 (9%) B | 71 (27%) B |
| 3 or more | 51 (58%) C | 4 (5%) A | 8 (9%) B | 16 (18%) C | 15 (19%) | 2 (2%) | 30 (34%) B | 11 (13%) B | 33 (38%) B |
| χ2 | 26.59**** | 9.10 * h | 10.67 * | 19.05 *** | 6.25 | 0.65 | 17.21 *** | 17.30 *** | 27.12 **** |
A–D Groups with the same superscript (A to D) within each row/column do not differ significantly.
a Physical health problem caseness was defined as Poor or Fair self-perceived physical health.
b Percentages with the same superscript within column within risk factor do not differ significantly.
c Depression caseness was defined as Moderate or Severe depression.
d Anxiety caseness was defined as Moderate or Severe anxiety.
e Somatic syndrome caseness was defined as Moderate or Severe somatic syndrome.
f Functional impairment caseness was defined as Moderate or Severe functional impairment.
g In order to reflect the analyses adjusting for Province, n and% are model-based estimates.
h Because of imbalanced cell sizes, the omnibus test in some instances may be significant but no pairwise comparisons significant.
i The Number of major storms line does not include 0 because n=5 for that cell.
j Number traumatic events includes traumatic major storm exposure.
For χ2 probability
* P<0.05
** P<0.01
*** P<0.001
**** P<0.0001.
Risk factors for mental health and life functioning problems
Gender was a risk factor for both mental and self-perceived physical health problems. Women had significantly higher rates of GAD and PTSD, and reported worse self-perceived physical health than men and greater life impairment related to mental health problems (Table 3). Men reported higher levels of alcohol dependence. Increasing age was associated with increased risk for all health conditions except alcohol dependence (Table 3). Conversely, education served as a protective factor for all health conditions except alcohol dependence (Table 3).
Higher levels of financial stress (Table 3) were a strong risk factor for all mental health domains except alcohol dependence, whereas the lifetime number of major storms experienced was not a significant predictor for any health condition (Table 3). Traumatic typhoon or other major storm exposure was associated with increased risk for self-perceived physical health problems, PTSD, and life functioning impairment. Lifetime number of traumatic events experienced (Table 3) was a significant risk factor for all health conditions except somatic syndrome and alcohol dependence.
Risk factor and mental health outcomes models
As noted above, we used canonical correlation analysisReference Tinsley and Brown 34 to assess overall relations between the (a) risk factors, and (b) health and life functioning outcomes. The overall relation between these two sets of variables was significant (F[105,5623]=5.66, P<0.0001), with the first three canonical correlations significant (all P<0.0001). In the first canonical relation (Fig. 1), the health outcomes canonical variate (i.e. the latent factor defined by the health outcome variables) represented poor overall health, with all outcomes (i.e. low self-perceived physical health, high mental health problems) except alcohol dependence contributing to the canonical variate. That is, all of the health outcome variables (physical health as assessed by the SF-36, depression as assessed by the PHQ-9, etc.) with the exception of alcohol dependence loaded on this canonical variate; it was labelled ‘poor’ health because the loading for (good) physical health was negative and the loadings for depression, etc., were positive. The risk factor canonical variate (upon which all of the risk factors potentially loaded) was defined primarily by higher financial stress and older age, and was related R 2=0.33 to overall poor health (i.e. the Poor Health canonical variate). Number of traumatic events contributed to the risk factor canonical variate but with a loading about 38% smaller than financial stress. Neither frequency of major storms nor exposure to a traumatic major storm contributed to the risk factor canonical variate.

Fig. 1 Canonical relation #1: risk factors for ‘Poor Overall Health'. The first canonical relation, between latent factors for (a) risk factors (as defined by the risk factor variables), and (b) health outcomes (as defined by the health and life functioning outcome variables, 'Poor Overall Health'). Variables loading 0.40 or higher within this canonical relation define their latent factor and are included in the figure. 'Physical health' refers to self-perceived physical health assessed using the Short Form Health Survey (SF-36) general physical health item.
In the second canonical relation (Fig. 2), the health outcomes canonical variate represented poor emotional mental health in the context of good self-perceived physical health (i.e. the SF-36 physical health item as well as the PHQ-9 and GAD-7 had positive loadings on this canonical variate, indicating that individuals high on this outcome canonical variate were reporting poor emotional mental health but good physical health). Again, the largest contributor to the risk factors canonical variate was financial stress, followed by age with a negative loading (i.e. younger individuals were higher on the health outcomes canonical variate representing poor mental health in the context of good self-perceived physical health). Alcohol dependence again was not a part of the health outcomes canonical variate. However, in the third canonical relation, the health outcomes canonical variate was defined by high levels of alcohol dependence (i.e. the only health outcome loading at or above 0.40 was alcohol dependence), and the risk factor canonical variate was defined by male gender (similarly, the only risk factor loading at or above 0.40 was male gender); that is, alcohol dependence was related to male gender, with no other health outcome or risk factors loading on the canonical variates (Fig. 3).
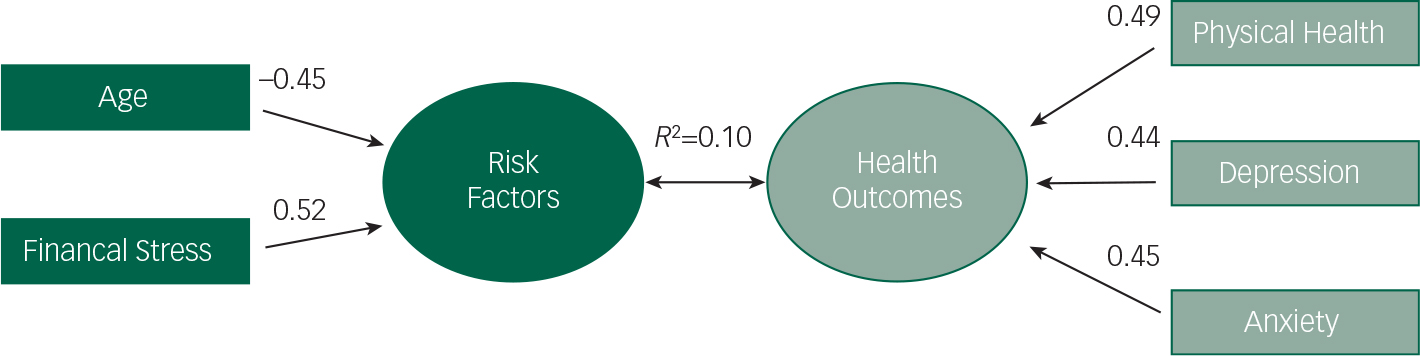
Fig. 2 Canonical relation #2: risk factors for ‘Poor Emotional Mental Health in the Context of Good Physical Health'. The second canonical relation, between latent factors for (a) risk factors, and (b) health outcomes (as defined by the health and life functioning outcome variables, Poor Emotional Mental Health in the Context of Good Physical Health; i.e. individuals high on this canonical variate have poor emotional mental health but good physical health). Variables loading 0.40 or higher within this canonical relation define their latent factor and are included in the figure. 'Physical health' refers to self-perceived physical health assessed using the Short Form Health Survey (SF-36) general physical health item.
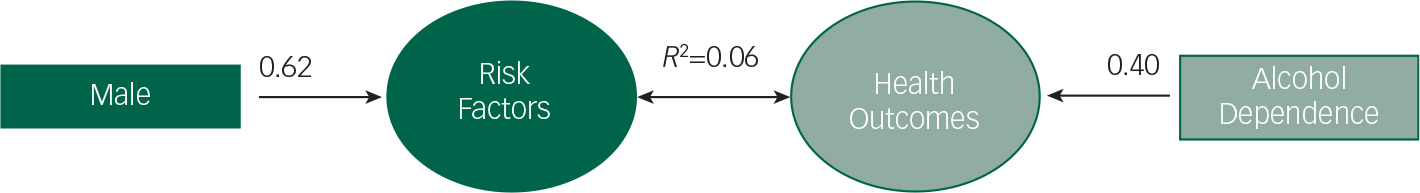
Fig. 3 Canonical relation #3: risk factors for 'Alcohol Dependence'. The third canonical relation, between latent factors for (a) risk factors, and (b) health outcomes. The only significant risk factor was male gender, and the only significant health outcome was alcohol dependence; that is, no other risk factors or health outcome variables loaded 0.40 or higher on their canonical variate.
Follow-up analyses
As one of the major findings from these analyses was that financial stress was a major predictor of mental health problems, we also assessed the relation between major storm exposure and financial stress. In this model, (a) financial stress was the dependent variable and (b) traumatic typhoon or other major storm exposure and number of storms experienced were the independent variables. This model was significant (F[2,931]=15.95, P<0.0001, R 2=0.03), with β=0.16 for traumatic major storm exposure, and β=0.09 for number of major storms experienced.
Discussion
The present study had two primary purposes: (a) to assess the mental health and life functioning status of individuals exposed to frequent natural disasters living in an LMIC context of chronic poverty, and (b) to determine the extent to which exposure to frequent typhoons and other major storms and related factors were associated with impaired health and life functioning. Based on our results, the central coastal Vietnam population does appear to be at increased risk for impaired life functioning, and physical and mental health problems, with 22% of the sample reporting moderate-to-severe functional impairment, 38% describing less than good (fair or poor) self-perceived physical health, and 23% reporting one or more significant mental health problem. Prevalence rates of current PTSD were high, with 10% of the sample meeting criteria. In contrast, a population-based study in Germany found a current PTSD prevalence rate of 1.7%,Reference Lukaschek, Kruse, Emeny, Lacruz, Rothe and Ladwig 35 and a study in Japan found a 12-month PTSD prevalence rate of 0.7% despite high rates (60%) of trauma exposure.Reference Kawakami, Tsuchiya, Umeda, Koenen and Kessler 36 In South Asia, a recent study of trauma and PTSD in Sri Lanka found a lifetime PTSD prevalence rate of 2.0%, also much lower than the 10% rate of current PTSD in our sample.Reference Dorrington, Zavos, Ball, McGuffin, Rijsdijk and Siribaddana 37 This does not appear to be due to overall level of economic development or trauma exposure. Although Germany and Japan are high-income countries, Sri Lanka is a lower-middle-income country as is Vietnam. Both Sri Lanka and Vietnam have a history of exposure to natural disasters as well as violence related to war but Sri Lanka's history of war is much more recent, suggesting that its PTSD rate should be higher. Although the Vietnamese sample in the current study had a higher rate of exposure to traumatic typhoons and other major storms (75% v. the Sri Lankan total trauma exposure rate of 36%), the twofold increase in trauma exposure probably does not explain the five-fold increase in PTSD.
Cultural factors, specific characteristics of the trauma, or methodological differences between studies are some factors that might explain the higher PTSD rate in our study. Various specific factors have been proposed for variations in prevalence rates of PTSD cross-nationally,Reference Hinton and Lewis-Fernández 38 including cultural beliefs regarding traumatic experiences that put people at greater or lesser risk for development of PTSD (e.g. the belief that traumatic events are due to karma, and deserved), and cultural differences in the way trauma-related psychological problems are experienced. For example, Cambodian refugees sometimes interpret nightmares (potentially a symptom of PTSD) to indicate depleted spiritual status or that one has been the victim of a spiritual attack, which could increase the physiological arousal and stress associated with nightmares and the likelihood of meeting PTSD criteria.Reference Hinton and Lewis-Fernández 38 , Reference Hinton, Hinton, Pich, Loeum and Pollack 39 Cultural syndromes thus may influence the interpretation of trauma-related symptoms and beliefs about long-term consequences of the trauma in ways that result in cultural variations in PTSD prevalence.Reference Hinton, Hinton, Pich, Loeum and Pollack 39 A more general social environmental factor that may play an important role in the development of PTSD, discussed by Hinton and Lewis-Fernández, is a person's level of chronic stress when exposed to the potentially traumatic (acute) event. Such background stress – including financial stress – could impact the development of PTSD through a chronically aroused HPA axis that consequently is more sensitive to acute traumatic events, leading in turn to increased rates of mental health problems.Reference Hinton and Lewis-Fernández 38
Rates of somatic syndrome in the Vietnamese sample were also high, with 16% of participants meeting criteria for moderate-to-severe somatic syndrome. In contrast, a meta-analytic review of mental health prevalence studies in Europe found a median 12-month prevalence rate for somatoform disorders of 4.9%.Reference Wittchen, Jacobi, Rehm, Gustavsson, Svensson and Jönsson 40 Prevalences of depression and anxiety (2% for moderate to severe depression; 5% for moderate to severe anxiety) in the Vietnamese sample, in contrast, were comparable to or lower than those of non-high-risk populations in Western countries. For instance, in Germany a population-based sample assessed using the same measures found prevalence rates of 5.6% for moderate–severe depression and 5% for moderate–severe anxiety.Reference Löwe, Decker, Müller, Brahler, Schellberg and Herzog 41
Arthur Kleinman was one of the first researchers to note high rates of somatic complaints in conjunction with low rates of affective symptoms among an Asian population.Reference Kleinman 42 Kleinman hypothesised that Asian people may tend to react to stressful life events in ways that emphasise somatic rather than affective symptoms because affective symptoms may be experienced by collectivistic Asian people as overly self-focused and consequently more disruptive to group harmony than somatic symptoms. Thus, the high rates of somatic syndrome in our sample in conjunction with low rates of emotional mental health problems may reflect such cultural values regarding non-expression of negative emotion, stigma related to affective mental illness, etc.Reference Lauber and Rössler 43 , Reference Chen, Cheung, Bond and Leung 44 A second interpretation comes from research on specific Vietnamese cultural somatic symptom syndromes.Reference Hinton, Hinton, Pham, Chau and Tran 45 Hinton and colleagues have suggested that somatic symptoms may be more common in certain cultures partly because they are a part of an organised idiom of distress recognised within that culture. When physiological arousal from stress results in somatic symptoms (e.g. trembling of the arms and legs), the symptoms may be conceptualised as part of an idiom of distress that becomes commonly recognised and accepted within certain cultures, thus increasing its prevalence. In Vietnam, there is a cultural understanding that somatic symptoms such as ‘chills’, ‘dizziness’ and symptoms characteristic of what is conceptualised as a panic attack in Western cultures may represent being ‘hit by the wind’. This particular cultural idiom of distress may therefore result in individuals in Vietnam who are experiencing high levels of both acute and chronic stress to be more aware and/or more likely to report such somatic symptoms, and increase its intensity by increased awareness. Finally, it is also possible that the relatively high rates of somatic syndrome reflected the relatively poor overall physical health in the sample. However, in the second canonical relation (Fig. 2) self-perceived physical health but not the somatic syndrome was part of the health outcomes canonical variate, suggesting that somatic syndrome is not synonymous with poor self-perceived physical health.
Alcohol use was common, particularly among men, with 87% of men reporting use of alcohol and 4% of the males (but no females) reporting symptoms of alcohol dependence. The primary predictor of alcohol dependence in this study was male gender. Alcohol dependence is related to male gender in Western countries but also to other factors as well, such as educational achievement, financial stress, trauma exposure, etc.Reference Merline, Jager and Schulenberg 46 None of these factors was related to alcohol dependence in the current study, however, which suggests that male gender roles may play a particularly important role in Vietnam in regards to alcohol dependence. In Vietnam, group binge drinking is a common social custom for men (‘di nhau’ in Vietnamese) that is seen as a part of masculine identity.Reference Nghe, Mahalik and Lowe 47 It thus may be particularly important for alcohol policy and abuse prevention efforts in Vietnam and similar LMIC to evaluate the impact of social gender-identity norms on alcohol use and abuse.
The second primary purpose of the present study was to determine whether increased exposure to relatively frequent natural disasters was associated with increased mental health and life functioning problems, to provide policy-makers and global health workers with important data for determining priorities and for planning purposes. In LMIC even moderately severe storms can cause significant destruction and disruption to people's life and livelihoods. Frequency of storm exposure and of traumatic storm exposure were elevated in this sample, with virtually the entire sample (99%) having experienced at least one major storm, more than 75% of people having experienced a traumatic major storm (i.e. fearing for his or her life or the life of loved ones, loss of a loved one or destruction of their home), and 86% having experienced at least one traumatic event (including a traumatic major storm). In comparison, a study conducted in Japan found that 60% of participants reported exposure to at least one traumatic event in their lifetime.Reference Kawakami, Tsuchiya, Umeda, Koenen and Kessler 36 A large epidemiological study from the United States found that 56% of people reported at least one lifetime traumatic event,Reference Kessler, Sonnega, Bromet, Hughes and Nelson 48 and a more recent population-based study in Germany found a lifetime rate of trauma exposure of 41%.Reference Lukaschek, Kruse, Emeny, Lacruz, Rothe and Ladwig 35
In our sample, the frequency of major storm exposure was not a significant predictor of any mental or self-perceived physical health problems assessed in this study whereas exposure to a traumatic major storm was. Individuals with traumatic typhoon or other major storm exposure showed an (a) 64% increase in poor self-perceived physical health, (b) 120% increase in risk for PTSD, and (c) 71% increase in risk for significant functional life impairment. However, the high prevalence of PTSD (10%) and overall mental health (23%) and functioning problems (22%) in our sample does not appear to be fully explained by traumatic major storm and other traumatic event exposure. In addition to major storms, this population also faces a number of other more chronic risk factors. Education is generally low, with a median education of the 8th grade. In our sample, one-third of the people were either unemployed or in unstable employment, with most people farmers or in other forms of unskilled labour. Approximately 30% of people reported moderate to high levels of financial stress. Low education, job uncertainty, financial stress, female gender, older age, farming as an occupation and previous exposure to trauma all predicted mental health and functioning problems. For instance, people with an elementary school education or less were about twice as likely to have a mental health problem as those people who had completed middle or high school. People who were unemployed or who had unstable work had higher rates of self-perceived health problems, depression, PTSD and greater life impairment, compared with people with stable employment. This is also a region in Vietnam that was exposed to violence during the Vietnamese civil war involving the United States. Our community sample reported a very low prevalence of war-related trauma exposure (<1%) probably because of the age of our sample relative to when the war ended (1975), although the war undoubtedly resulted in long-term economic impact and stress for the region.
Overall, however, financial stress was the strongest predictor of mental health problems, with 15% of individuals who reported low financial stress meeting criteria for one or more mental health problem, whereas 55% of individuals who reported high financial stress met such criteria. In fact, individuals reporting high levels of financial stress had the highest rate (55%) of mental health problems of any single risk category. Higher levels of financial stress also were associated with worse self-perceived physical health and greater functional impairment. Similar to other forms of chronic stress discussed above, the experience of financial insecurity as an ongoing threat may activate biological and psychological systems, increasing sensitivity to acute events and ultimately risk for various mental health problems.Reference Hinton and Lewis-Fernández 38
Global climate projections indicate increasing temperatures across Asia, predicted to lead to more intense tropical cyclones and increased risk of flooding and mudslides.Reference Field, Barros, Stocker, Qin, Dokken and Ebi 10 Southeast Asia is expected to have more days with intense rainfall.Reference Field, Barros, Stocker, Qin, Dokken and Ebi 10 Possible impacts include damage to homes, farmlands and other sources of livelihood, and the deterioration of community infrastructure and services.Reference Field, Barros, Stocker, Qin, Dokken and Ebi 10 Sea level rise is of particular concern for coastal areas such as that in the present study. Some meteorological and economic forecasts predict a sea level rise in Vietnam of up to 1 m by 2100, with a resultant 10% reduction of its GDP.Reference Tran 49 Even a much smaller sea level rise and reduction in GDP would have a profound impact on this region, as it contains a disproportionate number of low-income residents who are at especially high risk for effects of economic declines.Reference Kim 11 Gradual increases in storm frequency and severity related to global climate change are unlikely to be recognised as ‘natural disasters’ by governmental or meteorological agencies and may not directly result in increased mental health problem prevalence but still impact on mental health functioning indirectly, through their relation with increased economic stress as we found in the present study. Thus, preparations for global climate change in LMIC regions at increased risk for natural disasters should consider the mental health needs of the population. Similarly, these results also indicate that when supporting LMIC communities that have experienced a natural disaster, it will be important to consider the broader community context including poverty, in addition to the direct effects of the disaster. Additional research will be needed to evaluate specific effects of predicted climate change on economic functioning, and to more fully delineate its links to stress and mental health within these communities so that they may be most efficiently supported.
These problems are compounded by the fact that, in general, mental health services are absent or of poor quality in LMIC, including in Vietnam where there are few evidence-based intervention (EBI) mental health services available and few resources for training mental health providers in EBI services.Reference Weiss, Dang, Ngo, Pollack, Sang and Lam 50 The WHO Atlas study found that only 14% of low-income countries have psychosocial care available at most health facilities, and mental health-related policies are frequently lacking or ineffective, and community-level public health efforts often fail to consider mental health. 51 Thus, increasing economic and social stress related to climate change is occurring in the context of minimal mental health services at a time when the need likely will increase. Improving mental health services is particularly important considering that mental health problems place people at increased risk for impaired work and family functioning.
Limitations of the study should be considered. First, mental health syndromes were assessed based on clinical interview and self-reports but did not include independent medical assessments or observational measures. Second, the cross-sectional nature of the study limits our ability to draw causal inferences. Third, our study did not include culture-specific assessment tools. ICD and DSM diagnostic categories and criteria are often used clinically and in research in Vietnam, but culture-specific ways of experiencing and manifesting psychological symptoms (as suggested by the relatively high rates of somatic syndrome found in conjunction with non-elevated or low rates of affective disturbance) may make these categories and criteria incomplete in countries such as Vietnam.Reference Hinton and Lewis-Fernández 38 Finally, this study was conducted in one particular LMIC – Vietnam. Although it shares a number of characteristics with many other LMIC (e.g. high levels of poverty and low levels of education), it also undoubtedly differs in other ways (e.g. cultural factors), making it important for future research to examine relations between study variables in different LMIC.
In conclusion, individuals living in central coastal Vietnam have elevated rates of PTSD, somatic syndrome, functional impairment and relatively poor self-perceived physical health. Financial stress was the strongest predictor of mental health problems. Predicted global climate change potentially places communities such as this at significantly elevated risk for mental health problems through increased traumatic typhoon and other major storm exposure, and through indirect effects of less severe storm exposure on economic status but not directly through exposure to a general increased risk for typhoons and other major storms. Thus, disaster risk reduction and response efforts should consider pre-disaster community factors, such as economic conditions, in responding to and assessing the likely impact of disasters on community mental health and functioning.









eLetters
No eLetters have been published for this article.