Depression is highly prevalent in healthcare workers (HCWs). A recent meta-review including over 3.2 million HCWs determined that, since the COVID-19 pandemic, the prevalence of depression in HCWs is 14–37% globallyReference Chutiyami, Cheong, Salihu, Bello, Ndwiga and Maharaj1. Here, nurses were highlighted as having the highest prevalence of depressive symptoms compared with other HCW roles. The rate of suicide in nurses has been estimated to be 23% higher than the national average in the UK.Reference Windsor-Shellard2 Gilleen et alReference Gilleen, Santaolalla, Valdearenas, Salice and Fusté3 found that the prevalence of low mood, anxiety and stress symptoms in HCWs increased during the pandemic when compared with pre-pandemic measures, although recent evidence suggests that these changes may not be sustained in the general population.Reference Sun, Wu, Fan, Dal Santo, Li and Jiang4 Whether this increased prevalence will be sustained is yet to be determined, but any mechanisms that underlie such increases are important to recognise and address.
Depression incurs a significant personal cost to HCWs. In addition, healthcare organisations incur large financial costs as a result of mental health problems in their employees. The sickness absence rate of nurses, midwives and ambulance staff is roughly three to four times the national average for the labour force, and 20–30% of sick days in the UK National Health Service (NHS) are because of mental health problems.5,Reference Leaker and Debra6
Financial concerns and their association with depression
It is well established that low household income is associated with an increased risk of mental health problems.Reference Jitender Sareen7 The UK's Office for National Statistics (ONS) has highlighted the difference in the prevalence of depression in those who believe they have the ability ‘to afford an unexpected expense’ compared with those who do not.Reference Tim Vizard8 Evidence concerning the relationship between financial concerns and depression in HCWs is limited and comes from small studies with cross-sectional designs. An Italian study from 2020 reported a non-significant increased risk of depression for HCWs with income loss as a result of COVID-19.Reference Paolocci, Bussotti, Pompili, Muzi, Gambelunghe and Dell'Omo9 A previous study in a HCW population from Pakistan demonstrated an association between financial concerns and depression.Reference Sarfraz, Ji, Asghar, Ivascu and Ozturk10 A recent study from Afghanistan found HCWs who reported a low monthly income to be at higher risk of depression than those in higher wage brackets.Reference Mohammadi, Neyazi, Rangelova, Padhi, Odey and Ogbodum11
Study aims
To date, there has been no longitudinal exploration of how financial concerns have affected the mental health of HCWs. This is a highly topical issue given the ongoing pay disputes and strike action by HCW groups in the UK.Reference News12 We therefore conducted an analysis of data collected between December 2020 and October 2022 from the nationwide UK Research Study into Ethnicity and COVID-19 Outcomes in Healthcare Workers (UK-REACH) longitudinal cohort study.Reference Woolf, Melbourne, Bryant, Guyatt, McManus and Gupta13 This was a secondary analysis, the primary aim of which was to determine if financial concerns at baseline were associated with development of symptoms of depression at follow-up. Secondary aims were to determine if the prevalence of financial concerns among HCWs has changed over the course of the study, and to determine whether there are demographic or occupational predictors of developing financial concerns in HCWs.
Method
Overview
UK-REACH is a research programme that was established to investigate the disproportionate impact of the COVID-19 pandemic on HCWs from ethnic minority groups. In this work, we use data from the baseline questionnaire (administered December 2020 to March 2021) and the wave 4 questionnaire (administered June to October 2022, hereafter referred to as the ‘follow-up questionnaire’) of the prospective nationwide cohort study. We elected to examine the earliest and latest time points that we had data for because we expected that it would take considerable time for the effects of financial concerns to affect the mental health of participants. Furthermore, we wished to capture the effects of the UK's cost of living crisis on the prevalence of financial concerns. For a detailed overview of the study, see the study protocolReference Woolf, Melbourne, Bryant, Guyatt, McManus and Gupta13 and cohort papers.Reference Bryant, Free, Woolf, Melbourne, Guyatt and John14 All measures collected in the questionnaires are available in the data dictionary (https://www.uk-reach.org/data-dictionary).
Ethical approval
UK-REACH was approved by the Health Research Authority (Brighton and Sussex Research Ethics Committee; ethics reference number 20/HRA/4718). All participants gave informed written (electronic) consent. The UK-REACH study is registered at ISRCTN (reference: ISRCTN 11811602).
Involvement and engagement
We worked closely with a Professional Expert Panel composed of an ethnically and occupationally diverse group of HCWs, as well as with national and local organisations, to help shape the research question and analysis plan.Reference Woolf, Melbourne, Bryant, Guyatt, McManus and Gupta13 Two of the panel (S.L. and P.P.) are co-authors.
Study population
To be recruited into the cohort study participants had to be living in the UK, currently employed as a HCW or ancillary worker in a healthcare setting and/or registered with a participating UK healthcare regulatory body, and aged ≥16 years.Reference Woolf, Melbourne, Bryant, Guyatt, McManus and Gupta13
Recruitment
Recruitment into the study has been described in previous work.Reference Bryant, Free, Woolf, Melbourne, Guyatt and John14–Reference Woolf, McManus, Martin, Nellums, Guyatt and Melbourne19 In brief, participating healthcare regulators (for a list see the supplementary material available at https://doi.org/10.1192/bjo.2023.520) emailed their registrants to invite them to participate in the study. A small proportion of the cohort were recruited directly by hospital Trusts and advertising in newsletters/social media.Reference Bryant, Free, Woolf, Melbourne, Guyatt and John14 Those interested in participating accessed the study website, where they could provide informed electronic consent and complete the baseline questionnaire. Invitations to complete subsequent questionnaires were emailed to participants who provided consent.
Outcome measures and covariates
Screening for depression
Our primary outcome measure was meeting the screening threshold for depression on the Patient Health Questionnaire-2 (PHQ-2)Reference Kroenke, Spitzer and Williams20 at follow-up. The PHQ-2 comprises two questions concerning the frequency of low mood and anhedonia over the preceding 2 weeks, with each question being scored on a four-point scale from 0 (‘not at all’) through to 3 (‘nearly every day’). The sum of the scores from each question are combined to provide a single score (on a scale from 0 to 6). In the primary analysis, we use the validated cut-off point of ≥3 to indicate meeting screening criteria for depression.Reference Kroenke, Spitzer and Williams20 In a sensitivity analysis, we use the combined score as a continuous outcome measure.
Future financial concerns
Participating HCWs were asked the following question in both the baseline and the follow-up questionnaire, ‘How worried are you about your future financial situation?’, derived from questionnaire material developed as part of the Wellcome Trust's Longitudinal Population Studies COVID-19 questionnaire.21 This was supported by the Wellcome ‘Longitudinal Population Study COVID-19 Steering Group and Secretariat’ as a Strategic Support Science Grant (identifier 221574/Z/20/Z). Answers were on a five-point scale (1, ‘not at all’; 2, ‘a little bit’; 3, ‘moderately’; 4, ‘quite a bit’; 5, ‘extremely’). The measure collected at baseline was used to address the primary aim of the study (i.e. determining whether financial concerns predict the development of depression symptoms), and the measure collected in the follow-up questionnaire was used as an outcome measure in both secondary analyses (i.e. determining whether the prevalence of financial concerns has changed over the course of the study and whether there are particular occupational and demographic groups at risk of financial concerns).
Covariates
We adjusted for the following covariates in multivariable analyses: (a) demographic characteristics (age, sex assigned at birth, ethnicity), with ethnicity categorised according to the five broad ONS categories (White, Asian, Black, mixed, other);22 (b) occupation, collapsed into five categories (‘medical’, ‘nurses, nursing associates, midwives’, ‘allied health professionals and those in pharmacy, clinical sciences and optical roles’, ‘dental’ and ‘administrative/estates/other’Reference Martin, Pan, Melbourne, Teece, Aujayeb and Baggaley16,Reference Martin, Pan, Nazareth, Aujayeb, Bryant and Carr17,Reference Woolf, McManus, Martin, Nellums, Guyatt and Melbourne19 ) and (c) deprivation in residential area, as determined by the Index of Multiple Deprivation (IMD) quintile.24
These covariates are derived from information provided in the baseline questionnaire. We examine the association of the same variables in the analysis of occupational and demographic predictors of financial concerns at follow-up.
Statistical analysis
We excluded those with missing data for the primary outcome of interest (PHQ-2 at wave 4) and the primary exposure of interest (financial concerns at baseline), including those who answered ‘prefer not to answer’ to the relevant question. For the secondary analyses, we additionally excluded those with missing data on financial concerns at follow-up.
We summarised categorical variables with frequency and percentages, and non-normally distributed continuous variables with median and interquartile range. We used univariable and multivariable logistic regression to determine unadjusted and adjusted associations of financial concerns at baseline with meeting screening criteria for depression at follow-up. Multivariable analyses were adjusted for the all covariates above, as well as the PHQ-2 score at baseline. We presented the results as odds ratios or adjusted odds ratios (aORs), with 95% confidence intervals.
To investigate changes in financial concerns between the baseline and follow-up questionnaires, we examined a contingency table of these variables and tested whether the proportion in each outcome category remained consistent across the two time points, using a marginal homogeneity (Stuart–Maxwell) test.
To determine demographic and occupational predictors of financial concerns at follow-up, we used univariable and multivariable ordinal logistic regression. We tested the proportional odds assumption with the Brant test. Any violations were investigated by deriving binary variables for each cut-off point in the categorical outcome (i.e. not at all versus at least a little bit, not at all or a little bit versus at least moderately, etc.). We then fit logistic regression models with these as outcomes and plotted results to determine which variables violate the assumption.
We conducted two sensitivity analyses. In the first, we used univariable and multivariable linear regression (adjusted for the same covariates) to investigate whether examining the PHQ-2 score as a continuous outcome measure (rather than a binary measure) had any effect on the associations found in the logistic regression models used for our primary analysis. In the second, to investigate bias resulting from loss to follow-up, we compared the measures collected in the baseline questionnaire and used in the main analysis (sociodemographic, occupational, financial concerns and PHQ-2 score) in the cohort who did not respond to the follow-up questionnaire with those that did respond.
Multiple imputation by chained equations was used to impute missing covariate data in all models. The imputation model contained all variables except the one being imputed, including the outcome measure. Rubin's Rules were used to combine parameter estimates and standard errors from ten imputations into a single set of results.Reference Rubin23 Although indices of deprivation are available for UK countries outside England, these are not directly comparable with the English IMD.24 We therefore elected to code IMD data as missing for those outside England and impute the missing information.
All analyses were conducted with Stata version 17 for macOS (StataCorp, College Station, Texas, USA) Figures were drawn with GraphPad Prism (version 9.4.0 for macOS; GraphPad Software, San Diego, California, USA; www.graphpad.com).
Results
Formation and description of the analysed sample
Recruitment into the study and formation of the analysed sample is detailed in Supplementary Figure 1. A total of 15 199 HCWs provided a response to the baseline questionnaire. Of these, 3891 responded to the follow-up; 330 were excluded for not providing information on baseline or follow-up PHQ-2 items and/or the baseline financial concerns item, meaning that 3521 HCWs were included in the primary analysis (23.2% of those who responded to the baseline questionnaire). A further three HCWs did not provide information on their level of financial concerns at follow-up, therefore 3518 were included in the secondary analyses.
Median age was 48 (interquartile range 37–56) years, 74.8% were female and 22.7% were from ethnic minority groups. A total of 819 (23.3%) were employed in medical roles; 756 (21.5%) were registered nurses, midwives and healthcare assistants; and 1471 (41.8%) were allied health professionals or working in pharmacy, clinical sciences or optical roles. At baseline, 12.1% met screening criteria for depression and 56% were at least a little concerned about their future financial situation (Table 1).
Table 1 Description of the analysed cohort (N = 3521)
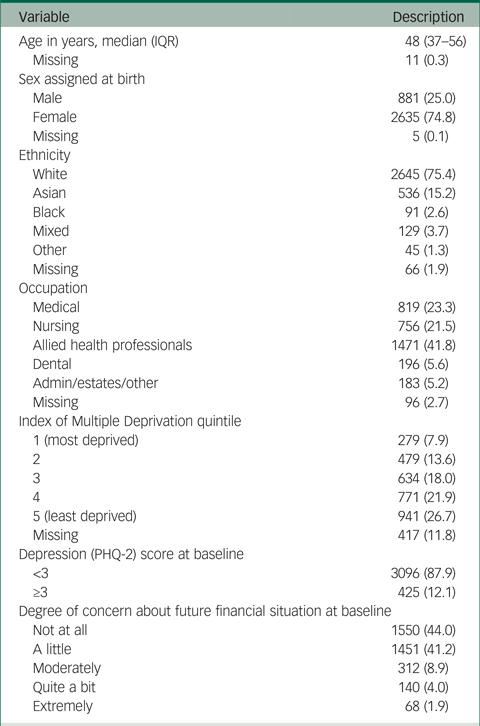
All data are n (%) unless otherwise stated. The nursing category includes healthcare assistants, nursing associates and midwives. The allied health professionals category includes healthcare scientists, ambulance workers, pharmacists and those in optical roles. IQR, interquartile range; PHQ-2, Patient Health Questionnaire-2.
Association of financial concerns and developing symptoms of depression
A description of the cohort stratified by the outcome measure (meeting screening criteria for depression at follow-up) together with unadjusted odds ratios for the association of each covariate with the outcome is shown in Table 2.
Table 2 Univariable analysis of the association between financial concerns and demographic/occupational factors at baseline with meeting depression criteria at follow-up
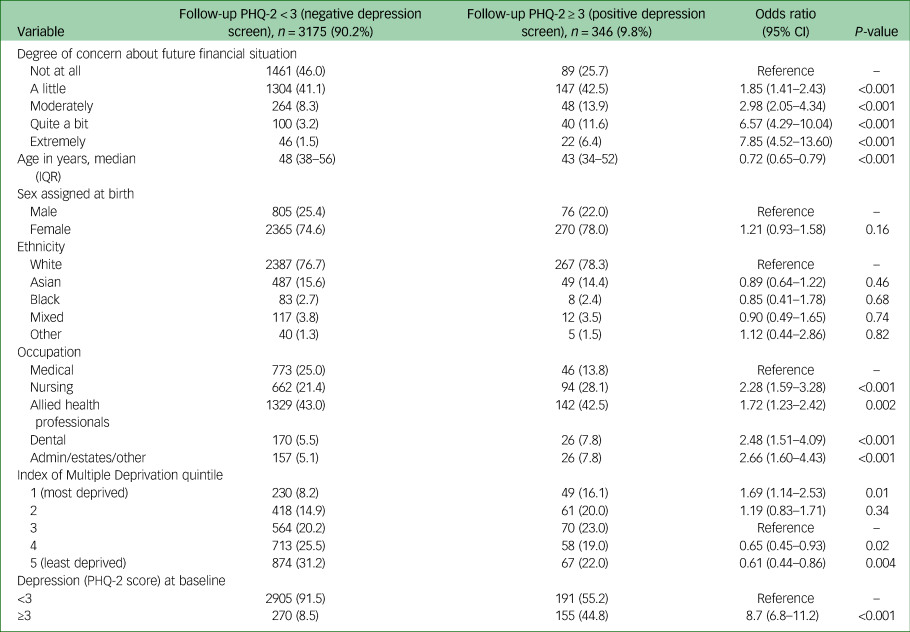
All data in the first two columns are n (%) unless stated otherwise; percentages are calculated column-wise, apart from the total number of those not meeting or meeting depression screening criteria, which are calculated row-wise. Odds ratios are from univariable logistic regression on the imputed data-set. Odds ratio for age is per decade increase. The nursing category includes healthcare assistants, nursing associates and midwives. The allied health professionals category includes healthcare scientists, ambulance workers, pharmacists and those in optical roles. PHQ-2, Patient Health Questionnaire-2; IQR, interquartile range.
The degree of participants’ concern about their future financial situation was strongly associated with meeting screening criteria for depression at follow-up. Those who were extremely concerned about finances at baseline had over seven times the odds of meeting the screening criteria for depression at follow-up compared with those who were not at all concerned at baseline (odds ratio 7.85, 95% CI 4.52–13.60).
After adjustment for age, sex assigned at birth, ethnicity, occupation, IMD quintile and baseline depression screening outcome (Fig. 1), greater future financial concerns at baseline were associated with higher odds of meeting screening criteria for depression (compared with not at all; a little: aOR 1.48, 95% CI 1.11–1.98; moderately: aOR 1.90, 95% CI 1.27–2.85; quite a bit: aOR 3.04, 95% CI 1.89–4.88; extremely: aOR 2.77, 95% CI 1.48–5.17). Increasing age was associated with lower odds of meeting screening criteria for depression at follow-up (aOR 0.84, 95% CI 0.75–0.94; per decade increase). Working in a nursing role compared with a medical role (aOR 1.61, 95% CI 1.05–2.47) was associated with higher odds of meeting screening criteria for depression at follow-up (see Fig. 1).
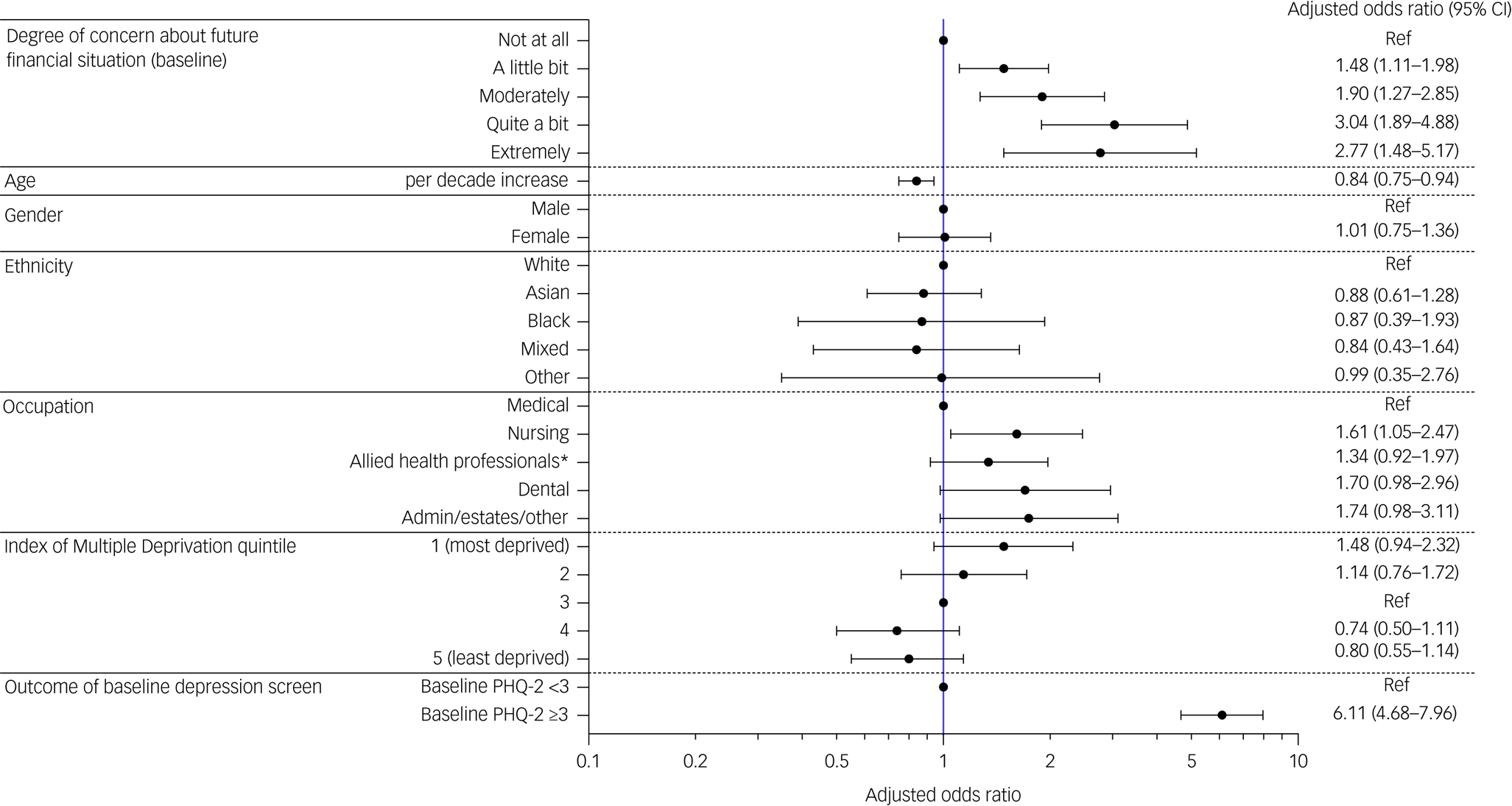
Fig. 1 Multivariable logistic regression demonstrating the relationship between financial concerns at baseline and meeting depression screening criteria at follow-up, after adjustment for demographics, occupation and baseline depression screening outcome. PHQ-2, Patient Health Questionnaire-2; Ref, reference group for categorical variable.
*Included in the 'Allied health professionals' group are healthcare scientists, pharmacists, ambulance workers and those in optical roles. Fig. 1 details the result of a mutivariable logistic regression analysis. Results are displayed as adjusted odds ratios (circles) and 95% confidence intervals (bars). Circles without bars are shown for the reference group of a categorical variable. Odds ratios are mutually adjusted for all variables in the figure.
Sensitivity analysis of PHQ-2 score as a continuous outcome using linear regression did not materially change the findings (see Supplementary Table 1).
Changes in financial concerns over time
A cross-tabulation of financial concerns at both time points is shown in Table 3: 44% reported no financial concerns at baseline compared with 22% at follow-up, 47.1% of the cohort reported the same level of financial concern at both time points, 43.8% reported an increased level of financial concern and 9% reported a decreased level of financial concerns at follow-up compared with baseline. The marginal homogeneity test was significant (P < 0.001), suggesting significant change in the proportion of HCWs concerned about their future financial situation between the two time points.
Table 3 Changes in the proportion of those with financial concerns between baseline and follow-up questionnaires
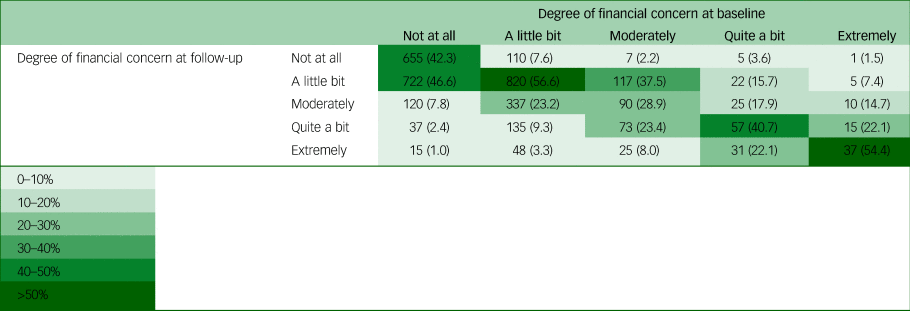
The table shows a cross-tabulation of the cohort by their responses to the financial concerns question at baseline (columns) and at follow-up (rows). All data are n (column %). Marginal homogeneity (Stuart–Maxwell) test P < 0.001.
Predictors of financial concerns at follow-up
Results of the univariable and multivariable ordinal logistic regression analyses to examine predictors of financial concerns at follow-up are shown in Table 4. After adjustment for age, sex assigned at birth, ethnicity, occupation, IMD quintile and baseline level of financial concerns, older HCWs had lower odds of having financial concerns (aOR 0.77, 95% CI 0.72–0.81). Those working in nursing or allied health professional roles (compared with medical roles) had higher odds of financial concerns at follow-up (nursing: aOR 2.28, 95% CI 1.84–2.82; allied health professional: aOR 1.64, 95% CI 1.37–1.97).
Table 4 Ordered logistic regression model demonstrating the univariable and multivariable association of demographic and occupational factors with increasing financial concerns at follow-up
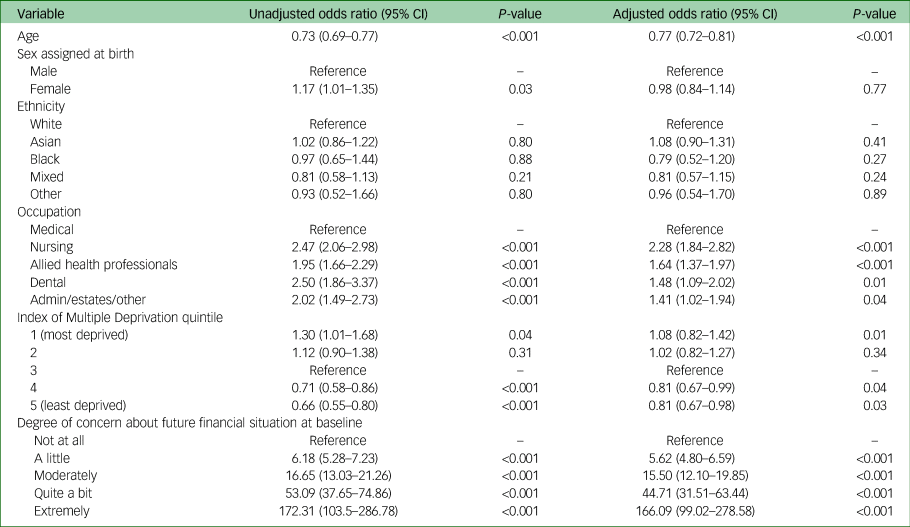
The table shows univariable and multivariable ordered logistic regression with an outcome of financial concerns at follow-up (five-level ordinal variable). Parallel odds assumption was checked with the Brant test. This was significant at P < 0.001. We plotted odds ratios derived from logistic regression for each level of the outcome variable and determined that the parallel odds assumption was likely violated by inclusion of baseline score. We tested this hypothesis by removing baseline score from the model and performing the Brant test again, which returned a non-significant P-value (see Supplementary Appendix 1). Given the importance of adjusting for baseline score, but the lack of importance placed upon the relationship of this variable with the outcome, we elected to continue with the planned analysis of using ordered logistic regression and adjusting for baseline score (accepting that the odds ratios for baseline score may not be accurate for all levels of the outcome variable). Odds ratio for age is per decade increase. The nursing category includes healthcare assistants, nursing associates and midwives. The allied health professionals category includes healthcare scientists, ambulance workers, pharmacists and those in optical roles.
For details of the post-estimation analysis of the validity of using ordinal logistic regression for this analysis, see Supplementary Appendix 1.
Investigating bias as a result of loss to follow-up
Compared with those that did not respond to the follow-up questionnaire, a higher proportion of those that responded had no financial concerns at baseline (36.6% v. 44%) and a lower proportion met the screening criteria for depression at baseline (15.3% v. 12.1%). Responders had a higher median age than non-responders, and a higher proportion of responders (compared with non-responders) were from White ethnic groups (76.8% v. 67.6%).
Discussion
In this analysis of a national cohort of 3521 HCWs, we found that those with financial concerns in December 2020 to March 2021 were more likely to develop symptoms of depression by June to October 2022 than those without such concerns. We also demonstrate that the proportion of HCWs concerned about their financial situation increased during the study period, with 43.8% reporting increased financial concerns and only 9% reporting decreased financial concerns. Predictors of developing financial concerns included younger age and working in a nursing or allied health professional role compared with a medical role.
Strengths of our study include the length of follow-up and large sample size. Ours is the first to use longitudinal data to examine the effect that financial concerns have on the risk of developing symptoms of depression in HCWs in the UK. Our work agrees with the existing literature. Sarfraz et al found an association between financial concerns and depression in a sample of HCWs in Pakistan.Reference Sarfraz, Ji, Asghar, Ivascu and Ozturk10 However, this study was limited by a small sample size, use of a non-standard depression screening tool and a cross-sectional design. In a USA cohort including (but not limited to) HCWs, financial concerns were associated with depressive symptoms.Reference Wilson, Lee, Fitzgerald, Oosterhoff, Sevi and Shook25 The ONS have determined that among British adults, prevalence of depression has increased between a pre-pandemic measure and early 2021 to a greater extent in those that indicated they were unable to afford an unexpected expense of £850 compared with those who could afford such an expense.Reference Tim Vizard8
Our study also has limitations. This questionnaire will likely suffer from response bias. Indeed our comparison of follow-up responders and non-responders indicates that those meeting the screening criteria for depression and those with financial concerns at baseline were less likely to respond to follow-up questionnaires (as has been described previouslyReference Biele, Gustavson, Czajkowski, Nilsen, Reichborn-Kjennerud and Magnus26), and this may have led to underestimates of the prevalence of depression and financial concerns. In comparison to the NHS workforce as a whole, our sample has a similar proportion of females and those from ethnic minority groups.27,28 The average age in our sample is higher than that of the NHS workforce,29 which could also have led to underestimates of the prevalence of financial concerns and depression. There are also some who may have left healthcare work as a result of financial concerns, depression or for other reasons. Inherent limitations exist in using a screening questionnaire to identify potential rates of depression. The PHQ-2 at a cut-off of ≥3 had a pooled sensitivity of 0.76 (95% CI 0.68–0.82) and a pooled specificity of 0.87 (95% CI 0.82–0.90), with substantial heterogeneity, in a 2016 meta-analysis.Reference Manea, Gilbody, Hewitt, North, Plummer and Richardson30 However, Löwe et al found that PHQ-2 change scores accurately reflected improved, unchanged and deteriorated depression outcomes in longitudinal data compared with the Structured Clinical Interview for DSM-IV (widely considered to be the gold standard for diagnosing depression in research).Reference Löwe, Kroenke and Gräfe31 The low numbers of particular specific occupational groups within the cohort necessitated combining particular groups (e.g. combining midwives with nurses and pharmacists with allied health professionals) to minimise exclusions and maximise statistical power. This may have introduced heterogeneity in some levels of the occupation variable, and may have led to the grouping together of those with relatively high and relatively low wage brackets. Finally, as with all observational studies, the relationship between exposure and outcome may have been affected by unmeasured confounding.
Increasing financial concerns and the associated depression found among HCWs could have several important consequences for the UK healthcare workforce and its staff, including negative effects on staff recruitment, retentionReference Poon, Lin, Griffiths, Yong, Seah and Liaw32 and sickness absence.Reference Copeland33 This could, in turn, lead to adverse consequences for patient safety, the workload of the remaining staff and waiting lists. In accordance with the existing literature, we find that working in a nursing role represents a risk factor for depression.Reference Chutiyami, Cheong, Salihu, Bello, Ndwiga and Maharaj1 Concerningly, we also find that among the different HCW occupational groups in this study, nursing staff had the highest odds of financial concerns by Autumn 2022. These findings suggest that increasing financial concerns could further widen the gap in depression prevalence between nurses and their colleagues in other healthcare roles.
NHS pay has not kept pace with the retail/consumer price index or the rate of inflation over the past decade, and the gap is likely to increase substantially over the next year,Reference Dayan and Palmer34 particularly compared with private sector pay in what is a competitive skilled labour market. Therefore, the prevalence of financial concerns among HCWs is likely to rise. The Nuffield Trust estimates that the average NHS employee has lost 4.5% of pay (adjusted for inflation) from 2010–2011 to 2021–2022. They also predict that, for starting nurses and doctors, respective real-terms pay losses will double, with first year doctors predicted to be paid 12.6% less in 2022–2023 than in 2010–2011.Reference Dayan and Palmer34 Compounding this problem is the current ‘cost of living crisis’ in the UK, which the Office for Budget Responsibility has predicted will worsen in 2023–2024.35
This real-terms pay cut has often been cited as a primary contributor to strike action across the NHS workforce (alongside increasing demand and work pressures).36–38 Currently, the government has no plans to increase pay to a level that would rectify the real-terms losses. For comparison, the Trades Union Congress estimates that financial and insurance sector pay has almost doubled since 2008,39 suggesting that public sector workers may be particularly afflicted by financial concerns.
Mental health problems, including depression, are consistently the most frequently reported reason for sickness absence in the English NHS, accounting for over 496 400 full-time equivalent days lost and 24.9% of all sickness absence.5 Sickness absence has previously been estimated to cost the NHS over £1 billion per year.Reference Jones40 There is also a large deficit in the supply of skilled labour, which means that even the current rate of 5% sickness affects the performance of the service and the experience of staff and patients. Despite this, little attention is given to pay, its relationship to well-being or the experience of worker's mental health in workforce policy. The NHS England People Plan and People Promise,41 published before the COVID-19 pandemic, aimed to address workplace cultures, but had no remit over pay. Historically, pay has been recognised as a retention lever but these data suggest it is also a performance lever in terms of the availability of staff and therefore services, and should be considered in workforce policy decisions. In our study, nursing appears to be the workforce where financial concerns and depression were most associated. Nursing has large-scale retention issues, with almost 50 000 unfilled posts in England,42 and this study suggests a much closer relationship between financial reward and depression than a straightforward reward and recognition issue.
In summary, a large and increasing proportion of UK HCWs in this large nationwide study were concerned about their financial situation, and this was associated with developing symptoms of depression. Those in nursing roles were at particular risk of developing financial concerns and depression symptoms. The relationship between financial concerns and depression among HCWs has concerning implications for the future of a healthcare workforce already plagued by understaffing, particularly in light of the current pay disputes and cost of living crisis in the UK. Further research should examine whether the relationship between financial concerns and subsequent depression observed in this study contributes to workforce attrition.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjo.2023.520
Data availability
To access data or samples produced by the UK-REACH study, the Working Group representative must first submit a request to the Core Management Group by contacting the UK-REACH Project Manager in the first instance. For ancillary studies outside of the core deliverables, the Steering Committee will make final decisions once they have been approved by the Core Management Group. Decisions on granting the access to data/materials will be made within 8 weeks. Third-party requests from outside the project will require explicit approval of the Steering Committee once approved by the Core Management Group. Note that should there be significant numbers of requests to access data and/or samples, then a separate Data Access Committee will be convened to appraise requests in the first instance.
Acknowledgements
We would like to thank all of the healthcare workers who took part in this study when the NHS was under immense pressure. We wish to acknowledge the members of the UK-REACH Professional Expert Panel (Amir Burney, Association of Pakistani Physicians of Northern Europe; Tiffanie Harrison, London North West University Healthcare NHS Trust; Ahmed Hashim, Sudanese Doctors Association; Sandra Kazembe, University Hospitals Leicester NHS Trust; Susie M. Lagrata (Co-Chair), Filipino Nurses Association UK and University College London Hospitals NHS Foundation Trust; Satheesh Mathew, British Association of Physicians of Indian Origin; Juliette Mutuyimana, Kingston Hospitals NHS Trust; Padmasayee Papineni (Co-Chair), London North West University Healthcare NHS Trust), the Steering and Advisory Group and Serco, as well as the following people for their support in setting up the study from the regulatory bodies: Kerrin Clapton and Andrew Ledgard (General Medical Council), Caroline Kenny (Nursing and Midwifery Council), David Teeman and Lisa Bainbridge (General Dental Council), My Phan and John Tse (General Pharmaceutical Council), Angharad Jones and Marcus Dye (General Optical Council), Charlotte Rogers (The Health and Care Professions Council) and Mark Neale (Pharmaceutical Society of Northern Ireland).
We would also like to acknowledge the following Trusts and sites who recruited participants to the study: Nottinghamshire Healthcare NHS Foundation Trust, University Hospitals Leicester NHS Trust, Lancashire Teaching Hospitals NHS Foundation Trust, Northumbria Healthcare NHS Foundation Trust, Berkshire Healthcare NHS Foundation Trust, Derbyshire Healthcare NHS Foundation Trust, South Tees NHS Foundation Trust, Birmingham and Solihull NHS Foundation Trust, Affinity Care, Royal Brompton and Harefield NHS Foundation Trust, Sheffield Teaching Hospitals NHS Foundation Trust, St George's University Hospitals NHS Foundation Trust, Yeovil District Hospital NHS Foundation Trust, Lewisham and Greenwich NHS Trust, Black Country Community Healthcare NHS Foundation Trust, Sussex Community NHS Foundation Trust, South Central Ambulance Service, University Hospitals Coventry and Warwickshire NHS Trust, University Hospitals Southampton NHS Foundation Trust, London Ambulance Trust, Royal Free, Birmingham Community Healthcare NHS Foundation Trust, Central London Community Healthcare NHS Trust, Chesterfield Royal Hospital NHS Foundation Trust, Bridgewater Community Healthcare NHS Foundation Trust, NHS Borders, County Durham and Darlington NHS Foundation Trust and Walsall Healthcare NHS Trust.
The UK-REACH Study Collaborative Group consisted of Manish Pareek (Chief Investigator), Laura Gray (University of Leicester), Laura Nellums (University of Nottingham), Anna L. Guyatt (University of Leicester), Catherine John (University of Leicester), I. Chris McManus (University College London), Katherine Woolf (University College London), Ibrahim Abubakar (University College London), Amit Gupta (Oxford University Hospitals), Keith R. Abrams (University of York), Martin D. Tobin (University of Leicester), Louise Wain (University of Leicester), Sue Carr (University Hospital Leicester), Edward Dove (University of Edinburgh), Kamlesh Khunti (University of Leicester), David Ford (University of Swansea) and Robert Free (University of Leicester).
Author contributions
M.P. conceived of the idea for UK-REACH and led the application for funding, with input from K.W. and the study collaborative group. The questionnaire was designed by C.A.M., K.W., M.P. and the study collaborative group. M.M., C.A.M., D.P., J.N., K.W. and M.P. formulated the idea for the analysis and contributed to the analysis plan, with input from L.T. and P.I. C.A.M. analysed the data, with input from L.T., K.W. and M.P. M.M., C.A.M. and M.B. drafted the manuscript with input, from S.L., P.P., D.P., J.N., A.L., K.W. and M.P. All authors reviewed, edited and approved the final version of the manuscript for publication.
Funding
UK-REACH is supported by a grant from the Medical Research Council UK Research and Innovation (grant MR/V027549/1) and the Department of Health and Social Care through the National Institute for Health and Care Research (NIHR) rapid response panel to tackle COVID-19. D.P. is an NIHR Doctoral Fellow (grant NIHR302338). K.W. was funded through an NIHR Career Development Fellowship (identifier CDF-2017-10-008) during the course of the study until December 2021. M.P. is supported by the NIHR Leicester Biomedical Research Centre (BRC) and NIHR Applied Research Collaboration East Midlands (ARC EM) and is funded by an NIHR Development and Skills Enhancement Award (number NIHR302865). This work is carried out with the support of BREATHE, the Health Data Research Hub for Respiratory Health (funding ID: MC_PC_19004), in partnership with SAIL Databank. BREATHE is funded through the UK Research and Innovation Industrial Strategy Challenge Fund, and is delivered through Health Data Research UK. This study was supported by the NIHR Applied Research Collaboration East Midlands and Leicester NIHR BRC. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. The funders had no role in study design, data collection, data analysis, interpretation or writing of the report.
Declaration of interest
M.P. reports grants from Sanofi, grants and personal fees from Gilead Sciences and personal fees from QIAGEN, outside the submitted work. K.W. is funded by the National Institute for Health and Care Research (Development and Skills Enhancement Award, NIHR302865) outside of this work, and has received funding from the NHS Race and Health Observatory outside of this work.









eLetters
No eLetters have been published for this article.