Dietary EPA and DHA intakes have been positively associated with improved endothelial function in young adults(Reference Leeson, Mann and Kattenhorn1). However, Egert et al.(Reference Egert and Stehle2) reviewed thirty-three intervention trials investigating the effects of n−3 PUFA on fasting and/or postprandial endothelial function and no clear conclusion could be drawn because of the small numbers in many trials and inconsistent methodology. The MARINA study (ISRCTN66664610) was a randomised controlled trial designed to test the hypothesis that increasing doses of EPA and DHA (0.45 g, 0.9 g and 1.8 g/d; equivalent to consuming 1, 2 or 4 portions of oily fish per week) taken for 1 year have favourable effects on endothelial function measured by flow-mediated dilatation (FMD) of the brachial artery. EPA+DHA and placebo (olive oil BP) were administered as supplements and the study was conducted double blind. A total of 367 non-smoking participants (142 men, 225 women aged 45–70 years, mean age 55 years) were randomised to treatment and a total of 312 subjects completed; data was available for analysis on 311 subjects for baseline and follow-up measurements of endothelial function. The mean (95% CI) increase in erythrocyte EPA compared with placebo was 0.74 (0.56–0.91), 1.31 (1.13–1.48) and 2.51 (2.33–2.69) wt % on 0.45 g/d, 0.9 g/d and 1.8 g/d, respectively (P<0.0001). Significant reductions in plasma TAG concentrations (P=0.002) were observed in women but not men: in comparison with placebo changes were −0.06 (−0.21 to 0.09), −0.12 (−0.27 to 0.03) and −0.29 (−0.44 to −0.14) mmol/l on doses of 0.45, 0.9 and 1.8 g/d, respectively. No significant treatment effects were noted for ambulatory blood pressure or arterial stiffness (pulse wave velocity). FMD was lower in men than in women (P<0.0001) and decreased with age (ρ=0.270; P<0.001) but there were no statistically significant treatment effects (P=0.781).
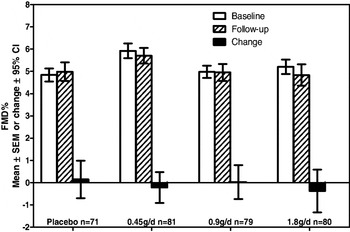
Our results are consistent with a cross-sectional survey in 3045 adults(Reference Anderson, Nettleton and Herrington3) that found no significant relationship between the n−3 LCP intake with FMD but a trend for FMD to be 0.1 and 0.27% lower on the highest compared with lowest intake in men and women, respectively. Our results indicate that intakes of n−3 LCP up to 1.8 g/d do not influence endothelial function in healthy non-smoking adults at moderate risk of CVD.
Funding for this work was provided by the Food Standards Agency and the Department of Health, England (Project code N02041).


