Obsessive–compulsive disorder (OCD) is a mental health problem associated with severe impact on quality of life.Reference Fontenelle, Fontenelle, Borges, Prazeres, Range and Mendlowicz1 Exposure and response prevention (ERP) is recommended as a first-line treatment for OCD, either as a monotherapy or in combination with medication.Reference Koran, Hanna, Hollander, Nestadt and Simpson2 ERP has been shown to be a very effective treatment. A review of 37 cognitive–behavioural studies found effect sizes of 1.3 (compared with waiting-list or placebo).Reference Ost, Havnen, Hansen and Kvale3 Unfortunately, 31% of patients drop-out of ERP treatment prematurelyReference Mancebo, Eisen, Sibrava, Dyck and Rasmussen4 and others do not fully adhere to ERP.Reference Simpson, Marcus, Zuckoff, Franklin and Foa5 The degree of patient adherence to ERP is significantly associated with the degree of improvement.Reference Simpson, Marcus, Zuckoff, Franklin and Foa5, Reference Abramowitz, Franklin, Zoellner and DiBernardo6 Low adherence results in less improvement, less remission and, as a consequence, higher relapse rates.Reference Eisen, Sibrava, Boisseau, Mancebo, Stout and Pinto7
The need to understand and address ambivalence in OCD
One explanation of drop-out and non-adherence is that patients with OCD are ambivalent about treatment,Reference Simpson and Zuckoff8 which means that they simultaneously want to change and are reluctant to change.Reference Miller, Arkowitz, Arkowitz, Miller and Rollnick9 This ambivalence is expressed in their choice to enter therapy, but not to adhere to treatment instructions. Ambivalence is described in the transtheoretical model of change,Reference Prochaska10 which distinguishes five successive stages in changing behaviour: pre-contemplation, contemplation, preparation, action and maintenance. According to this model, patients move from the pre-contemplation stage, in which they have no intention to change, to the contemplation stage, which is characterised by ambivalence and arguments in favour of and against change. While moving from the contemplation stage to the preparation stage, more arguments favour change, whereas fewer argument oppose change.Reference Prochaska10 During the preparation stage, an individual intends to take action in the immediate future. During the action stage, individuals actually change their behaviour. The stages of this model are dynamic, in the sense that patients not only progress though the stages sequentially, but may also fall back to previous stages.Reference Prochaska10 ERP for OCD usually involves several behavioural changes (usually described in an ‘exposure hierarchy’11), which means that patients move through the stages of the transtheoretical model every time they change an aspect of their obsessive–compulsive behaviour. Addressing patients' ambivalence about treatment is therefore crucial throughout treatment.
Interventions designed to enhance motivation
Interventions designed to enhance motivation, such as motivational interviewingReference Miller and Rollnick12 and thought mapping,Reference Meyer, Souza, Heldt, Knapp, Cordioli and Shavitt13 are used to help patients with OCD resolve this ambivalence and succeed in treatment. In motivational interviewing the patients' own motivation for change is evoked by the therapist, who facilitates their ‘statements that favour change’ by ‘seeking to evoke, understand, reflect, explore and summarise it’.Reference Miller, Arkowitz, Arkowitz, Miller and Rollnick9 Motivational interviewing is used in the treatment of substance dependence,Reference DiClemente, Corno, Graydon, Wiprovnick and Knoblach14 anxiety disorders, depression, eating disordersReference Westra, Aviram and Doell15 and several other disorders.Reference Lundahl, Moleni, Burke, Butters, Tollefson and Butler16 Thought mapping is another motivation technique. It is based on the transtheoretical model of changeReference Prochaska10 and is used to organise the patients' thoughts and behaviours and may help them to consider solutions for their problems.Reference Meyer, Souza, Heldt, Knapp, Cordioli and Shavitt13
Besides motivational interviewing and thought mapping, the use of home videos of OCD compulsions could be a tool to deal with the ambivalence to change. We use such videos in the in-patient treatment programme of our department. The initial goal of these videos was to provide the therapist with information about the compulsions of the patient (for example about their content, frequency, duration and consequences). Clinical observations, however, suggested that the use of these videos had additional effects on the patients' motivation. Especially at times when treatment progress stagnated, watching their home video appeared to give patients additional motivation to continue their exposure exercises.
A possible explanation for this enhanced motivation could be that they became acutely aware of their compulsive behaviours by seeing them on video, which seemed to help them realise that they needed treatment. According to the transtheoretical model, being aware of one's behaviour and its consequences is important in the first stages of this model.Reference Prochaska10 Watching their home video seemed to help patients reflect on their behaviour and thereby to enhance their motivation for treatment.
Use of video recordings in other mental illnesses
As far as we know the use of videos of patients' compulsive behaviour has not been studied previously. A few studies have been published on using self-made videos of patients, but these involved other mental illnesses. In psychotic disorders, Davidoff et al Reference Davidoff, Forester, Ghaemi and Bodkin17 and Virkam et al Reference Vikram, Yarger, Coxell and Maier18 found improvement of insight after watching a video of their own behaviour when they had psychotic symptoms. Another study, however, could not confirm this finding.Reference David, Chis Ster and Zavarei19 In social anxiety disorder, video feedback is used to correct the distorted self-perception.Reference Rapee and Hayman20–Reference Harve, Clark, Ehlers and Rapee22 In anorexia nervosa, Probst et al Reference Probst, Vandereycken and Van Coppenolle23 used videos to improve patients' attitude about their bodies. OthersReference Mihai, Damsa, Allen, Baleydier, Lazignac and Heinz24–Reference Paredes, Ludwig, Hassenfeld and Cornelison26 used video confrontation in patients with alcohol dependence to improve their insight into how they behave when they are intoxicated. Mihai et al Reference Mihai, Damsa, Allen, Baleydier, Lazignac and Heinz24 conducted an RCT in which 60 patients with alcohol dependence were randomised; they reported that patients who watched the videos (n = 30) had a significantly lower relapse rate. Geertsma & ReivichReference Geertsma and Reivich27 used video confrontation for a female patient with a personality disorder.
Study aims
This study aimed to answer the following questions: (a) how do patients respond to watching home videos of their personal compulsive rituals? and (b) do patients report an effect on motivation for treatment, and if so, can we formulate hypotheses about how watching home videos affects motivation for treatment? In addition to these questions, we focused on identifying potentially adverse events. Given the exploratory nature of this research, we conducted a qualitative study focused on the experiences of the patients. By carefully listening to patients, hypotheses can be formulated that can be tested in future quantitative studies.Reference Pope and Mays28, Reference Corbin and Strauss29
Method
Study design
We conducted an exploratory pilot study with a qualitative observational design using two semi-structured interviews that were intended to identify the effect of watching videos of personal compulsive rituals in patients with OCD who were being treated with ERP in an in-patient programme.
Ethics
The study was accredited by the ethics committee (METiGG). All participants gave written informed consent. We were concerned that the videos could provoke feelings of despair with possible consequences such as suicidal thoughts. We therefore, carefully asked all patients whether they experienced such feelings. To ensure close observation we limited our research to patients who participated in an in-patient programme. We also conducted a second interview after 6 weeks to discuss any adverse events and to determine whether the videos had any effects on the participants that were not mentioned during the first interview.
Participants
Twenty-four adult participants (15 women and 9 men) were included in the study and participated in the first interview. Their mean age was 37.9 (s.d. = 9.5). Their mean total score on the Yale-Brown Obsessive Compulsive ScaleReference Goodman, Price, Rasmussen, Mazure, Fleischmann and Hill30 was 23.8 (s.d. = 5.1) (obsessions 11.8, s.d. = 4.2, compulsions 12.1, s.d. = 3.1). All participants received in-patient treatment (from Sunday evening until Friday afternoon) for OCD in a specialised clinic. In the Netherlands, in-patient treatment is available for patients with treatment-resistant OCD who did not respond to adequate out-patient treatment with serotonergic antidepressants and ERP. All participants were diagnosed according to DSM-IV-TR31 criteria by experienced clinicians. The only inclusion criterion was OCD with overt compulsions that could be filmed. To ensure maximum variation sampling, we did not apply exclusion criteria.
From November 2010 until December 2013, 32 patients were asked to make a video as part of their treatment, of these 6 refused. Of the 26 patients who made a video, 1 refused to participate in the present study. Another participant was excluded, because no compulsions were visible on his video. Twenty participants took part in the second interview: four patients dropped out (three because of logistical reasons and one terminated treatment prematurely). Patients were included until additional interviews did not add new information.Reference Corbin and Strauss29
Procedure
As part of our treatment programme, all patients admitted to our intensive in-patient programme were visited at home by our nursing staff. These visits were planned in the first weeks of the 6-month treatment. During these visits, the nurses listed the compulsions that the patients performed at home. Together with the nurse, patients selected some compulsions to be recorded on video to provide their therapist with relevant information. Patients were instructed to perform these compulsions as usual, which were recorded for about 20 min. Severity of OCD symptoms was assessed using the Yale-Brown Obsessive Compulsive Scale to characterise the study sample.
To ensure confidentiality, participants watched their video with, and were interviewed by, a staff psychiatrist who was not involved in their treatment. During the interview they were encouraged to be open about any positive and negative aspects of watching the videos. Some questions were designed to elicit negative reactions. (For example, ‘It is a hassle to make and watch these videos, is it worth the effort?’). The interviewer frequently made summaries and reflection statements to confirm understanding of the participants' responses.Reference Britten, Pope and Mays32 After the first interview, which lasted about 20–50 min, the videos were used in the regular treatment. Six weeks after the first interview, a shorter second interview (10 min) was held.
Materials
Two interviews were developed. Based on a standard approach in qualitative research, the interviews were semi-structured using open-ended questions to discover the participants' experiences and to avoid influencing them with the researcher's assumptions.Reference Britten, Pope and Mays32, Reference Kelley, Bourgealt, Dingwall and de Vries33 Initial questions focused on how participants experienced watching their home video and what kinds of feelings were elicited by watching the video. Questions about the usefulness of the videos and effects on their motivation were asked later in the interview to avoid shaping participants' responses and to allow them to bring up these elements themselves.
As confrontation with their compulsions might evoke feelings of despair, if they did not mention such feelings spontaneously, we asked patients whether they experienced these feelings. When this was not the case, we asked them if they could imagine that others would have these feelings and why they did not have such feelings themselves. Some participants expressed feelings of despondence or despair. We carefully explored these feelings and checked whether suicidal ideation emerged. Finally, participants were asked whether they felt that all aspects were discussed.
The goal of the second interview was primarily to discuss any adverse events and to determine whether the videos had any effects on the participants that were not mentioned during the first interview. At the end of this second interview, as a member check (respondent validation),Reference Mays and Pope34 to enhance the internal validation of the study, patients were given a summary of the first interview and asked whether the summary was correct and if they had anything to add.
To develop and refine hypotheses as the study progressed, we used the acquired data to formulate new questions.Reference Corbin and Strauss29, Reference Charmaz35, Reference Pope, Ziebland, Mays, Pope and Mays36 For example in the second interview we asked whether the patients experienced flashbacks of the video. All such changes and additions to the interview were discussed in the research team.
Analysis
The entire process, from study design to coding and writing up the results, was discussed and refined in regular meetings with the research team. This team consisted of three psychiatrists (H.J.G.M.v.M., A. S. de Leeuw,, J.A.M.d.M.) and five psychotherapists (H.A.D.V., M. J. B. G. Bartels, N. Y. Spijksma, M.F.R.v.G.-d.V.v.S., B. M. L. Bringmans); experienced in working with patients with OCD. All interviews were recorded and transcribed verbatim. The transcripts were then coded with a combination of thematic codingReference Pope, Ziebland, Mays, Pope and Mays36 focused on motivation and adverse events, and open codingReference Corbin and Strauss29 for all the other content of the interviews. To reduce researcher bias by means of investigator triangulation,Reference Patton37 all interviews were coded by several researchers. A coding scheme for the first and second interview was developed by five researchers (H.J.G.M.v.M., J.A.M.d.M., M.F.R.v.G.-d.V.v.S., N. Y. Spijksma, M. J. B. G. Bartels), who analysed the transcripts of the first five interviews. The subsequent 19 interviews were coded twice by two researchers (J.A.M.d.M. and M.F.R.v.G.-d.V.v.S.). Based on a grounded theory approach,Reference Corbin and Strauss29, Reference Charmaz35 the transcriptions were read and re-read and phrases were coded. Through constant comparison of new data with the emerging understanding, codes were interpreted, summarised, redundant codes deleted and overlapping codes merged. Newly emerging themes were added to the coding process and applied to the previously analysed interviews. Discrepancies in coding between J.A.M.d.M. and M.F.R.v.G.-d.V.v.S. were discussed and resolved by consensus.Reference Patton37 The codes were grouped into clusters based on the main subthemes that emerged. ‘Deviant cases’ were sought to challenge the emerging themes.Reference Corbin and Strauss29, Reference Mays and Pope34, Reference Charmaz35 Coding was facilitated by MAXQDA software (http://www.maxqda.com/).
Quotations are used to illustrate the described themes; to identify the participant's quotations we used the participant's number.
Results
Coding of the first and second interview
Open coding of the first interview revealed four themes summarised in the following subsections: ‘Enhanced insight and awareness’, ‘Emotions elicited by the video’, ‘The desire to change’ and ‘How watching videos enhances insight, awareness and the desire to change’. Thematic coding on motivation is described together with the open coding results of ‘the desire to change’. Open coding of the second interview is described in: ‘effects of the video at follow-up’.
Thematic coding on adverse events is described in a separate section. An overview of the results is presented in Table 1.
Table 1 Overview of results as expressed by the participants during the first interview

Y-BOCS, Yale-Brown Obsessive Compulsive Scale.
a. Doubt, doubt whether they will be able to improve.
Enhanced insight and awareness
Most of the participants (92%, n = 22) reported aspects of OCD of which they had been unaware, such as: repeated actions (38%, n = 9), long duration and slowness (29%, n = 7) and irrational behaviour (38%, n = 9).
‘Then I think “goodness, that's a bit much”. There I go, wiping behind the faucet with the cloth again. I can't help thinking, “hang on I've done that ten times already”. Do I really do it so many times? That's excessive.’ (P-8)
Nine participants (38%) mentioned signs of progress they had already made in their treatment.
‘That was already better, more relaxed, acceptable. Good, I thought it was good. That's something I've learned. Take it easier. That's something that keeps coming back to me.’ (P-2, commenting on how he cleaned the table.)
Most participants (79%, n = 19) mentioned the impact on their lives. They talked about exhaustion and the time-consuming aspects of OCD. Ten (42%) mentioned the impact on others, such as children (29%, n = 7), parents (13%, n = 3), spouse (4%, n = 1) and relatives (8%, n = 2).
‘I'm constantly washing my hands. This goes on the whole day. I'm thinking: “how can I live this way”.’ (P-1)
Emotions elicited by the video
Most participants (67%, n = 16) experienced transient negative feelings. Such as sadness (58%, n = 14), shame (25%, n = 6), irritation (25%, n = 6), anger (25%, n = 6), tiredness (17%, n = 4), a bit despairing (13%, n = 3), a bit despondent (13%, n = 3), loneliness (8%, n = 2), restlessness (4%, n = 1) and guilt (4%, n = 1). Feelings of ‘a bit despairing’ and ‘a bit despondent’ were experienced while facing up to the seriousness of their OCD, wondering if they would be able to change (83%, n = 5 of the participants who experienced these feelings).
‘Another feeling that comes up is very paradoxical, it is despondency. It's the futility of “bringing water to the sea”. Facing up that is tough. I have the feeling that I can't improve, but where are you then.’ (P-20)
The desire to change and motivation
Most participants (92%, n = 22) indicated that watching the video made them want to change their compulsions.
‘Yes… yes, so this has got me thinking again… about all those things I do at home. Yes… yes, yes, that I don't want things to be that way and… that I really want to change things.’ (P-10)
Nineteen (79%) of them mentioned specific goals.
‘Yes, I can see that situation now. I see all those things in the kitchen and how I move around. I'm able to think of small steps I can take. For example, not trying to keep as far away from the door as possible [to prevent contamination]. It makes it more practical. It's something I can work on.’ (P-14)
Some participants (33%, n = 8) used the word ‘motivating’ spontaneously in relation to the video. Others (21%, n = 5) agreed when the interviewer used this word. One used the word ‘encouraging’ and one talked about ‘enhanced commitment’.
‘Yes, absolutely it motivates me. I think it helps to see the repetition. I think that next time when I clean, I will think about the video it and try to do it once.’ (P-11)
Eighteen participants (75%) emphasised ambivalent feelings when they realised that they wanted to change, but that changing was difficult. Six (25%) of them expressed doubt that they would be able to change.
‘How strong is my will? How strong is my desire to let go a lot of behaviour.’ (P-16)
On the other hand, 17% (n = 4) of the participants said that they could not imagine that they would not improve, and one participant even argued that it would not be very difficult to achieve improvement.
‘It's made things clear in a different way and then it seems more ridiculous. And I don't think it would be difficult to change.’ (P-15)
How watching videos enhances insight, awareness and the desire to change
Most participants (92%, n = 22) elaborated on how they gained a greater insight into their symptoms and became more motivated to change by watching the video. They mentioned three themes:
(a) ‘Being an observer’ rather than a participant, leading to more insight and awareness (92%, n = 22).
(b) Insight and awareness made it ‘difficult to ignore the seriousness’ of their compulsions (58%, n = 14).
(c) Seeing progress on the video shows that treatment works (25%, n = 6).
Figure 1 provides a graphical representation of these themes.
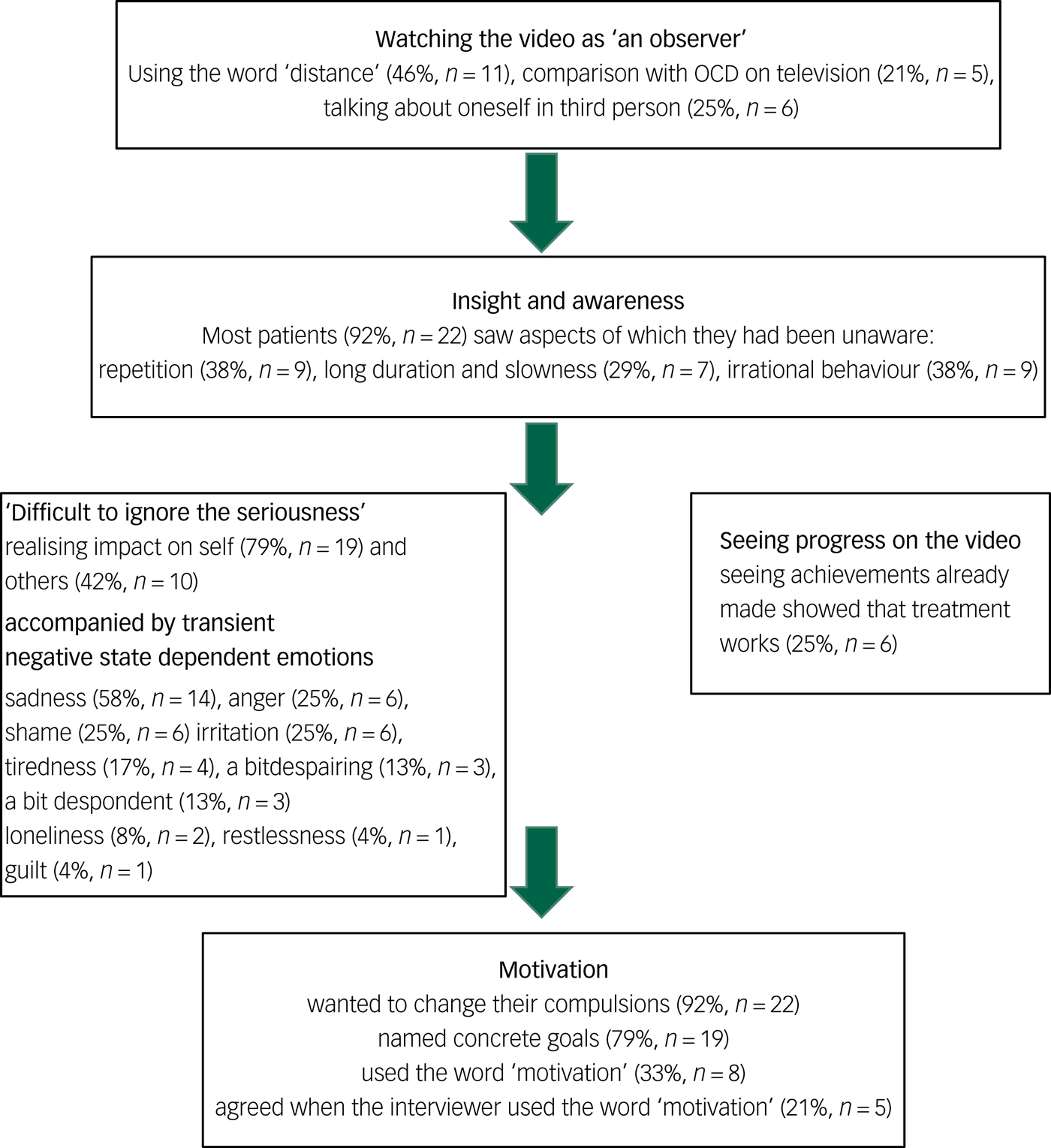
Fig. 1 Graphical representation of the themes.
Being an observer
Participants (92%, n = 22) mentioned that when they perform their compulsions they experience a great deal of tension, anxiety and a diminished sense of time and of their surroundings. While watching their video they were not bothered by these factors and were able to observe and reflect on their behaviour.
‘When you're in the middle of it, you're caught up in what you're doing and it alters your sense of time. Then you look at the clock and see that an hour has elapsed though it only feels like a few minutes.[…] When you're not involved in that compulsive behaviour, you can see what you're actually doing.’ (P-9)
Participants (46%, n = 11) frequently used the word ‘distance’ to describe this state of ‘being an observer’; they said that watching their video was as if they were watching someone else. This ‘distance’ is also illustrated by the fact that some participants (21%, n = 5) made comparisons between their behaviour and what they had seen about OCD on television. Others (25%, n = 6) referred to themselves in the third person, and one said that her behaviour looked like she was working with radioactive material, instead of laundry.
‘Without doubt it helps to take distance towards your own behaviour. It gives extra motivation to change when you look at it from a distance and when you see how serious it really is and how much time it takes up. That can help you feel more motivated.’ (P-6).
Three participants (13%) reported increased awareness of sounds. For example, one of them reported that while she watched her video she heard sounds indicating that her door was really closed. During the making of the video she had not noticed these sounds.
Difficult to ignore the seriousness
Many participants (58%, n = 14) emphasised that watching the videos made it difficult to trivialise their behaviour. Enhanced insight and awareness (38%, n = 9) and a stronger connection with their feelings (33%, n = 8) were cited as factors that made it difficult to deny that their OCD is a serious problem and increased their motivation to change.
‘Now you're forced to face the facts, you are seeing it yourself. Instead of only feeling the anxiety, or getting rid of the anxiety by compulsive washing.’ (P-3)
Seeing progress on the video shows that treatment works
Some participants (25%, n = 6) reported that the video not only showed them the futility and severity of their OCD but, after seeing the achievements they already had made in treatment, it also showed that treatment works.
‘When you see that it's successful, you're more inclined to keep going because you know it works.’ (P-12)
Effects of the video at follow-up
Many participants had thoughts about the video (75%, n = 15), especially when performing the compulsions they observed in the video (50%, n = 10). Some of them even were able to visualise the video images while thinking about the videos (40%, n = 8). Their thoughts about the video were frequently accompanied by thoughts about specific changes to improve (55%, n = 11). They reported that these thoughts were helpful to change (45%, n = 9).
‘I've been thinking about it a lot. In the video I see a compulsive person and I don't want to be that way. That's an enormous help. I think “Oh no…” and I picture the video and think “That's not what I want” and that helps me stop my compulsive behaviour.’ (P-24)
Although the participants were not asked whether watching the video actually changed their behaviour, 13 (65%) spontaneously reported improvement. Nine (45%) viewed this as a result of watching their video. Participants also reported; enhanced motivation (15%, n = 3), increased awareness (15%, n = 3), better insight (20%, n = 4), and greater perseverance in stopping the compulsions (5%, n = 1). Others felt stronger (5%, n = 1), encouraged (5%, n = 1) and hopeful (5%, n = 1). Two participants (10%) said that initially they had been focused on making gradual progress, and after watching the video they had decided to try to rid themselves of OCD completely.
‘It made me stronger, in the sense that I really want to get rid of these rituals and the obsessive counting. I can't work any harder at it, but now I realise that it is not normal, I want to get rid of it. Before I thought that I would be glad with a little improvement, but now I want to get rid of it completely; that is my goal, washing my hands without counting and rituals.’ (P-19)
Adverse events
Although participants expressed transient negative feelings, none reported feelings of severe sadness or despair or suicidal thoughts. When asked why they thought they did not develop these feelings they referred to the progress they already made (25%, n = 6), stated that they already knew that their OCD was severe (13%, n = 3), emphasised that realising the severity of their OCD would be positive because they want to change (8%, n = 2) and referred to their choice for treatment (8%, n = 2).
Discussion
Main findings
The first aim of the present study was to describe how patients respond to watching home videos. Nearly all participants reported seeing aspects of their OCD that they had been unaware of, for example, the amount of repetition. Before watching the video, they apparently did not know in detail what the content of their compulsions was. ‘Watching their compulsions as an observer rather than a participant’ was described by the participants as helpful to gain more insight. The participants described a high level of tension and stress when they engaged in their compulsions. When they observed their compulsions on the video, however, they experienced less tension and stress. This helped them to see what was really happening. Realising what really happened made it difficult to ignore the seriousness of their compulsions and evoked transient negative feelings such as sadness, shame and irritation.
The second aim was to determine whether there was an effect on motivation. Patients reported to be motivated for change; 92% (n = 22) of the participants indicated that watching the video made them want to change, 79% (n = 19) mentioned specific goals, 33% (n = 8) named motivation spontaneously and another 21% (n = 5) agreed about feeling motivated. In summary, after watching the videos many participants reported increased insight, which created transient negative state-dependent emotions that enhanced their motivation to change.
We expected that being confronted with their compulsions as shown on the video might evoke feelings of despair, that could result in serious side-effects. We therefore focused on identifying potentially adverse events. However, other than transient negative feelings, no serious adverse events were reported.
Interpretation of our findings
The relationship between acquiring more insight into obsessive–compulsive symptoms and increased motivation to engage in ERP is in accordance with the transtheoretical model of change.Reference Prochaska10 Moving from the contemplation stage to the preparation stage is characterised by an increase in arguments in favour of change and a decrease in arguments against change.Reference Prochaska10 According to the participants, watching the videos enhanced their insight into and awareness of the seriousness of their OCD, which helped them to find arguments in favour of change and dismiss arguments against change. For example, patients found arguments in favour of change when talking about the impact of their compulsions on their lives, the impact on the lives of others and the irrationality and severity of their compulsions. The next stage, the preparation stage, usually involves a plan of action. In the interviews participants talked about specific treatment goals. Setting such goals belongs to the preparation stage and could help them to progress to the action stage.
The way participants talked about the videos has much in common with motivational interviewing. According to the motivational interviewing approach, a therapeutic relationship that facilitates working together is based on acceptance, partnership, compassion and evocation (‘Calling forth the client's own wisdom, values, ideas and plans.’Reference Miller, Arkowitz, Arkowitz, Miller and Rollnick9). In this therapeutic relationship, the patients' motivation to change was elicited by asking open questions, affirming the patients' strengths, using reflection and summarising.Reference Miller, Arkowitz, Arkowitz, Miller and Rollnick9 The therapeutic relationship described in motivational interviewing resembles the approach taken in the present study: watching the videos together with the participants, regarding them as experts in their own behaviour and feelings, not judging the behaviour on the video, and asking primarily open questions to ensure a credible qualitative interview. Watching the videos together resulted in talking about wanting to change, motivation, ambivalent feelings and doubt. Other researchers have hypothesised that motivational interviewing works because patients verbalise the disadvantages of their problematic behaviour, the advantages of changing this behaviour and their ability and intention to change (change talk).Reference Miller, Arkowitz, Arkowitz, Miller and Rollnick9, Reference Miller and Rollnick12 During this change talk, ambivalence is resolved in the direction to change.Reference Miller, Arkowitz, Arkowitz, Miller and Rollnick9 Related studies have shown that the ratio of change talk versus sustain talk (‘speech that defends the status quo’Reference Miller, Arkowitz, Arkowitz, Miller and Rollnick9) predicts the likelihood of change.Reference Moyers, Martin, Houck, Christopher and Tonigan38, Reference Moyers, Martin, Christopher, Houck, Tonigan and Amrhein39 In the present study, after watching the videos the patients engaged in a lot of ‘change talk’, which could cause more motivation and change.
Besides resemblances, there are also some differences between the approach in the present study (watching and discussing the video) and motivational interviewing. At first, watching the video seemed to enhance insight and awareness. Nearly all participants reported becoming aware of specific aspects of their compulsions, and most of them started to talk about the impact of OCD on their lives. This seemingly prevented denial of the seriousness of the compulsions. Participants mentioned this as a reason to change. In motivational interviewing, clinicians actively respond to change talk, but in our study we only asked how watching the videos was experienced without paying specific attention to change talk. This change talk emerged spontaneously. Watching the video and using motivational interviewing techniques could possibly evoke even more change talk.
The present study shows that videos can be used in ERP to enhance motivation, but they could also be used in many other ways, for example to register expression and frequency of symptoms and avoidances, as a form of exposure and so on.
Limitations
Our study has several limitations. First, all participants were undergoing treatment as part of our in-patient programme, which reduces the external validity. Second, we only included patients with compulsive behaviour that could be recorded on video. This also reduces the external validity, because we did not include patients with only mental compulsions. We do have some clinical experience with using videos with patients with mental compulsions, by asking them to express their mental rituals verbally. According to these clinical observations, such interventions might also enhance motivation. Third, we used the video within the first weeks of treatment. It is possible that the effect of the videos differs depending on the phase of treatment (early/middle/late) in which they are used.
Implications and directions for future research
The present study shows that watching home videos with compulsions, seem to have encouraging effects on motivation. ‘Watching their compulsions as an observer rather than a participant’ was described as helpful. As this was an exploratory pilot study, we did not measure motivation using motivation questionnaires. In future studies, we advise the use of quantitative measurements of motivation. It would also be interesting to use the videos in other samples of patient's with OCD, to use the videos repeatedly in all phases of treatment, and to find out if videos of mental compulsions and reassurance seeking can also be used. Another promising line of research would be to study the use of videos and motivational interviewing together. The potential effects of watching the videos on insight and awareness might increase the effects of motivational interviewing, and in turn motivational interviewing might increase the effect of watching the videos because in motivational interviewing the clinician actively evokes and strengthens change talk.Reference Miller, Arkowitz, Arkowitz, Miller and Rollnick9
There are lots of other psychiatric disorders, such as depression, anxiety disorders and psychotic disorders in which insight and motivation are also important for treatment. It would be beneficial to find out whether videos also enhance motivation in these disorders and to find out if observing their complaints ‘as an observer rather than a participant’ could also be helpful in these disorders.
Funding
This research was supported by a grant from MIND Netherlands (grant no. 20106477).




eLetters
No eLetters have been published for this article.