Introduction
Fontan-Kreutzer univentricular circulation involves a total cavopulmonary anastomosis, characterised by the absence of a subpulmonary ventricle. This surgical procedure enables individuals with a functionally univentricular heart to sustain life, although it is accompanied by chronically elevated systemic venous pressure and a variable degree of reduced cardiac output. Reference Kreutzer, Lugones, Kreutzer and Kreutzer1 Reference Rychik, Atz and Celermajer,2
Notably, the thoracic duct empties into the left jugular-subclavian vein junction, and the persistent elevation in systemic venous pressure associated with Fontan-Kreutzer univentricular circulation may impede normal lymphatic drainage. Reference Kreutzer and Kreutzer3 Recently, advancements in non-invasive imaging technologies, particularly magnetic resonance imaging utilising T2-weighted sequences without external contrast enhancement, have facilitated the visualisation of the lymphatic system. Consequently, monitoring for lymphatic anomalies in individuals with functionally univentricular circulation is now recommended. Reference Rychik, Atz and Celermajer2 Lymphatic abnormalities that are particularly associated with failing Fontan-Kreutzer circulation, such as protein-losing enteropathy and plastic bronchitis, have been documented. Reference Dori, Keller and Foller4
Pulmonary hypertension in univentricular circulation is defined by a transpulmonary gradient exceeding 6 mmHg (calculated as the mean pulmonary artery pressure minus the mean left atrial pressure or pulmonary artery wedge pressure), and/or a pulmonary vascular resistance index exceeding 3 Wood units per square metre. Reference Del Cerro, Abman and Diaz5 Per the World Symposium on Pulmonary Hypertension, pulmonary hypertension in the setting of univentricular circulation is categorised as group 5, owing to its unclear and/or multifactorial aetiology. Reference Hansmann, Koestenberger and Alastalo6 It is noteworthy that the concept of pulmonary hypertension differs for individuals with univentricular circulation compared to those with biventricular circulation, as even a mean pulmonary artery pressure of 20 mmHg may exert significant effects on systemic veins and the lymphatic system. Reference Rychik, Atz and Celermajer2 Pulmonary artery remodelling is considered a risk factor in the postoperative care of Fontan-Kreutzer patients, with reports of organised pulmonary thrombus formation with recanalisation. Reference Juaneda and Haworth7
Lymphatic abnormalities have previously been documented in pulmonary hypertension in the setting of biventricular circulation (group 1), particularly in the presence of right ventricular failure. Reference Juaneda, Catalfamo and Fregapani8 To the best of our knowledge, there are no magnetic resonance lymphangiography findings in Fontan-Kreutzer univentricular circulation that have been found to be associated with transpulmonary gradient and functional phenotype.
Methods
Following approval from the ethical committee, informed consent was obtained from all participants (January 2017 through October 2019). Inclusion criteria comprised patients with Fontan-Kreutzer univentricular circulation who underwent both magnetic resonance lymphangiography and cardiac catheterisation. A total of seven patients met these criteria, and a summary of their demographics is presented in Table 1. The mean age of the cohort was 16.57 ± 7.10 years, and the cohort consisted of five males and two females. Two-dimensional-Doppler transthoracic echocardiography assessments revealed a diagnosis of single ventricle with left ventricular morphology in four patients and right ventricular morphology in three. Atrioventricular valve competence was observed in five patients, while incompetence was noted in two patients with hypoplastic left heart syndrome. The Fontan-Kreutzer procedure was conducted at an average age of 6.85 ± 2.89 years, with closure of extracardiac tube fenestrations performed in all patients at the time of the study. Given the absence of a standardised functional classification for patients with univentricular circulation, we adopted the biventricular Panamá paediatric pulmonary hypertension functional class classification for patients younger than 16 years and the World Health Organization adult functional class classification for those older than 16 years. Reference Lammers, Adatia and Del Cerro9 Patients #1, #2, and #3, who did not exhibit pulmonary hypertension, were classified as functional classes I–II and were in good clinical condition. Conversely, the remaining patients were classified as functional class IIIa, IIIb, or IV, with two patients diagnosed with protein-losing enteropathy, one with plastic bronchitis and heterotaxy syndrome, and two with heart failure. The mean systemic oxygen saturation was 87.7 ± 3.4%.
Table 1. The white panel indicates a transpulmonary gradient ≤ 6 mmHg in patients without pulmonary hypertension, while the grey shadowed panel indicates a transpulmonary gradient>6 mmHg in patients with pulmonary hypertension
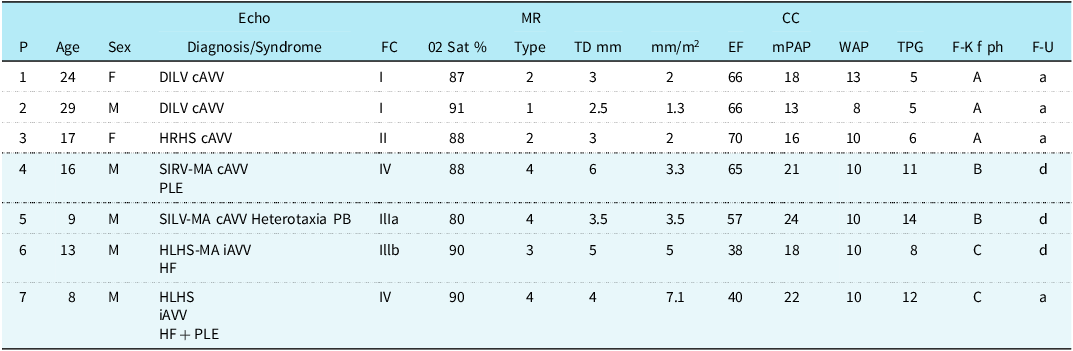
Abbreviations: P = patient number, Y = years of age, F = female, M = male, Echo = echocardiography, DILV = double inlet left ventricle, cAVV = competent atrioventricular valve, iAVV = incompetent atrioventricular valve, HRHS = hypoplastic right heart syndrome, SILV = single inlet left ventricle, MA = mitral atresia, PLE = protein-losing enteropathy, PB = plastic bronchitis, HLHS = hypoplastic left heart syndrome, FC = functional class, O2 Sat.% = oxygen saturation percentage, MR = magnetic resonance, TD = thoracic duct diameter/index, EF = ejection fraction, CC = cardiac catheterisation, mPAP = mean pulmonary artery pressure, mLAP = mean left atrial pressure, WPAP = wedge pulmonary artery pressure, F-K f ph = Fontan-Kreutzer function phenotype: A = functional class I-II, competent atrioventricular valve, lymphangiography type 1-2 with preserved ejection fraction and transpulmonary gradient ≤6 mmHg; B = functional class III- IV, competent atrioventricular valve, lymphangiography type 4 with preserved ejection fraction and transpulmonary gradient>6 mmHg; C = functional class III-IV, incompetent atrioventricular valve, lymphangiography type 3-4, with decreased ejection fraction and transpulmonary gradient>6 mmHg, F-U = follow-up, a = alive, d = dead.
Results
Table 1 presents the results, demonstrating that patients with lymphatic abnormalities categorised as type 1 or 2 and a transpulmonary gradient ≤ 6 mmHg exhibited a normal functional phenotype (Category A, represented by white shaded rows). Conversely, patients with lymphatic abnormalities categorised as type 3 or 4 and a transpulmonary gradient >6 mmHg exhibited a Fontan-Kreutzer failure phenotype (Categories B or C, represented by grey shaded rows). Lymphangiography comparisons between patients with and without pulmonary hypertension revealed the following findings: qualitative lymphatic abnormalities were predominantly categorised as type 1 or 2 in patients without pulmonary hypertension, whereas those with pulmonary hypertension exhibited primarily type 3 or 4 abnormalities. Additionally, quantitative analysis demonstrated a smaller thoracic duct diameter (2.8 ± 0.20 mm vs. 4.6 ± 0.90 mm, p = 0.0323) and index (1.76 ± 0.30 mm/m2 vs. 4.42 ± 1.55 mm/m2, p = 0.0323) in patients without pulmonary hypertension and a higher quantitative ejection fraction of 67.3 ± 1.88% versus 50.00 ± 11.30% (p = 0.0323).
Cardiac catheterisation revealed that patients with pulmonary hypertension had higher transpulmonary gradients (11.25 ± 2.16 mmHg vs. 5.33 ± 0.47 mmHg, p < 0.0323) and mean pulmonary artery pressures (21.25 ± 2.16 mmHg vs. 15.66 ± 2.05 mmHg, p = 0.0497), with no differences in pulmonary artery wedge pressure, mean left atrial pressure, or univentricular end-diastolic pressure (10.00 ± 0.0 mmHg vs. 10.30 ± 2.05 mmHg, p = 1.000).
Based on functional class, atrioventricular valve competency, magnetic resonance lymphangiography, univentricular ejection fraction and transpulmonary gradient, three distinct Fontan-Kreutzer functional phenotype categories were delineated: A) Normal, characterised by functional class I or II, competent atrioventricular valve, lymphangiography type 1–2 with preserved ejection fraction and transpulmonary gradient ≤ 6 mmHg; B) Failure, characterised by functional class IIIa or IV, competent atrioventricular valve, lymphangiography type 4 with preserved ejection fraction and transpulmonary gradient >6 mmHg (indicative of pulmonary hypertension); and C) Failure, characterised by functional class IIIb or IV, incompetent atrioventricular valve, lymphangiography type 3–4 with decreased ejection fraction and transpulmonary gradient >6 mmHg (also indicative of pulmonary hypertension).
Survival analysis from the time of the Fontan-Kreutzer operation to November 2023 indicated a higher survival rate (3/3) among patients with lymphangiography type 1–2 and transpulmonary gradient ≤ 6 mmHg with median duration of follow-up of 18.1 (interquartile range, 13.3–26.5) years, compared to those with lymphangiography type 3–4 and transpulmonary gradient >6 mmHg, with follow-up duration of 7.4 (interquartile range, 6–10) years, where only 1/4 patients survived and 3/4 died with a follow-up duration of 6.6 (6–7) years.
Consequently, based on these mortality rates, patients with functional phenotype A were deemed to have low-risk determinants, whereas those with functional phenotype B or C were considered to have high-risk determinants.
Discussion
Patients #1, #2, and #3 shared common features of lymphangiography types 1–2 and transpulmonary gradient ≤ 6 mmHg (Figure 1), while patients #4, #5, #6 and #7 exhibited lymphangiography types 3–4 and transpulmonary gradient >6 mmHg (Figures 2 and 3). Integration of functional class, echocardiography, magnetic resonance lymphangiography, ejection fraction and cardiac catheterisation transpulmonary gradient enabled the characterisation of three distinct functional phenotypes in patients with Fontan-Kreutzer univentricular circulation: A, B or C.

Figure 1. Patient #2 magnetic resonance lymphangiography type 1, normal functional phenotype A.

Figure 2. Patient #4 magnetic resonance lymphangiography type 4, failing phenotype B.
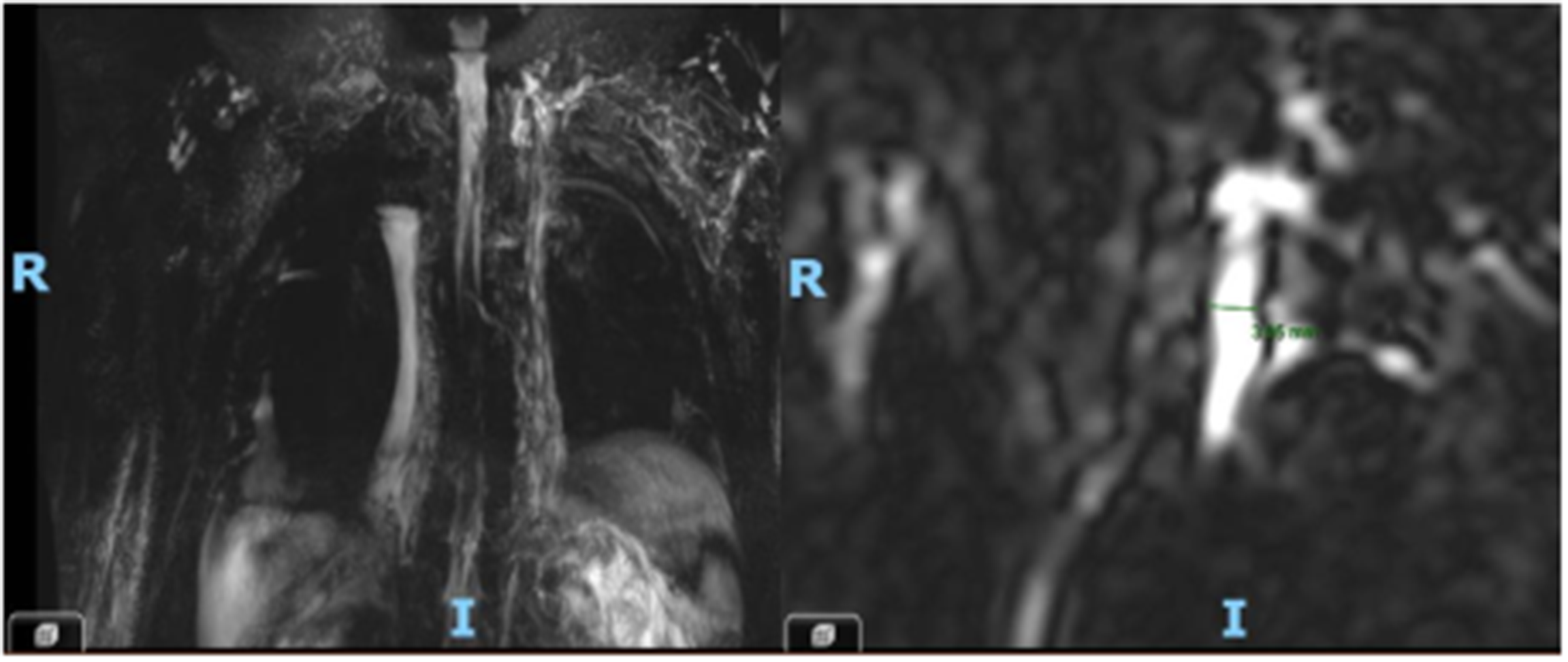
Figure 3. Patient #6 magnetic resonance lymphangiography type 3, failing phenotype C.
Should our findings be validated in larger studies, further investigation into how lymphangiography features could enhance risk stratification in this population would be warranted. All patients in this study exhibited mild cyanosis, suggesting a potential induction of endothelial dysfunction. Reference Krimly, Jain and Egbe11 Reference Senavirathna, Huang and Pusbparai,12
For patients #4 and #5 with failing phenotype B, it is speculated that the pathophysiology of pulmonary hypertension may be attributed to pulmonary vascular disease, stemming not only from cyanosis-induced pulmonary arteriolar endothelial dysfunction but also from non-pulsatile pulmonary flow and mechanical/inflammatory processes associated with possible silent/chronic pulmonary thrombosis/thromboembolism. Reference Juaneda, Catalfamo and Fregapani8,Reference Sathananthan, Johal and Verma13,Reference Laflamme and Roche14
Conversely, patients #6 and #7 with failing phenotype C may have pulmonary hypertension secondary to left-sided heart disease and similar contributing factors of phenotype B.
A recent publication describing the pathophysiology of the lymphatic system in heart failure with biventricular circulation describes an increase in thoracic duct flow via the following mechanisms: “1) elevated venous pressures generate an excessively high flux of water into the interstitial space; and 2) removal of interstitial fluid and its return to the venous system (including flow through the thoracic duct) is impeded by elevated central venous pressure.” Notably, these factors likely explain the lymphatic abnormalities seen in patients with univentricular circulation secondary to chronic increased systemic venous pressure, leading to clinical manifestations of organ-specific congestion. Reference Itkin, Rockson and Burkhoff15
Maintenance of patients with Fontan-Kreutzer univentricular circulation in phenotype A would bode well for survival.
Despite the identification of these functional phenotypes associated with findings on magnetic resonance lymphangiography, the sample size of this study is small and as such, the implications of the study are limited. Nonetheless, this represents an avenue for future research.
Conclusion
Magnetic resonance lymphangiography in patients with Fontan-Kreutzer univentricular circulation and pulmonary hypertension revealed qualitative lymphatic abnormalities of type 3–4, indicative of a failing functional phenotype compared to patients without pulmonary hypertension. If validated in larger studies, these results suggest the potential utility of this extracardiac biomarker for improving risk stratification in this population. Integration of lymphangiography and transpulmonary gradient with functional class, atrioventricular valve function, and ejection fraction allowed for the categorisation of three distinct functional phenotypes, which may be valuable for future analyses.
Acknowledgements
The authors extend their gratitude to: Joav Dori, MD, PhD - Children’s Hospital of Philadelphia, for his generosity in teaching static magnetic resonance lymphangiography; Shahin Moledina, MD - Great Ormond Street Hospital, for his kindness in instructing magnetic resonance real-time cineangiography ejection fraction techniques; Marcela Ruiz Funes, PhD - Georgia Southern University, for her thorough English review of this manuscript, and Eduardo Cuestas, MD, PhD - National University of Córdoba, for his statistical revision of this manuscript.
Financial support
This case report received no financial support.
Competing interests
All authors affirm the absence of any conflicts of interest.
Ethical standard
This case report has obtained approval from the Ethics Committee.
Guarantor
Not applicable.







