102 results
Impaired health-related quality of life, and depressive symptoms in a cohort of healthy adults with symptoms of attention deficit/hyperactivity disorder
-
- Journal:
- European Psychiatry / Volume 68 / Issue 1 / 2025
- Published online by Cambridge University Press:
- 03 March 2025, e44
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Prevalence and comorbidity rates of disruptive mood dysregulation disorder in epidemiological and clinical samples: systematic review and meta-analysis
- Part of
-
- Journal:
- European Psychiatry / Volume 68 / Issue 1 / 2025
- Published online by Cambridge University Press:
- 15 January 2025, e11
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Surge in antidepressant usage among adolescents and young adults during the COVID-19 pandemic: insights from an interrupted time series analysis
-
- Journal:
- Epidemiology and Psychiatric Sciences / Volume 33 / 2024
- Published online by Cambridge University Press:
- 07 November 2024, e62
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Gender differences in the relationship between depressive symptoms and diabetes associated with cognitive-affective symptoms
-
- Journal:
- BJPsych Open / Volume 10 / Issue 6 / November 2024
- Published online by Cambridge University Press:
- 05 November 2024, e192
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Electroconvulsive therapy response and remission in moderate to severe depressive illness: a decade of national Scottish data
-
- Journal:
- The British Journal of Psychiatry / Volume 225 / Issue 6 / December 2024
- Published online by Cambridge University Press:
- 18 September 2024, pp. 547-555
- Print publication:
- December 2024
-
- Article
-
- You have access
- HTML
- Export citation
Chapter 16 - Inflammation and Metabolic Issues in Mood Disorders
-
-
- Book:
- Clinical Textbook of Mood Disorders
- Published online:
- 16 May 2024
- Print publication:
- 23 May 2024, pp 163-171
-
- Chapter
- Export citation
Association of clinical variables and thyroid-stimulating hormone with psychotic symptoms in patients with first-episode and drug-naïve major depressive disorder with elevated fasting blood glucose: preliminary exploratory study with a large sample
-
- Journal:
- BJPsych Open / Volume 10 / Issue 3 / May 2024
- Published online by Cambridge University Press:
- 03 May 2024, e99
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
A retrospective analysis of iv ketamine outcome on hospitalisations in an unselected psychiatric sample
-
- Journal:
- Acta Neuropsychiatrica / Volume 37 / 2025
- Published online by Cambridge University Press:
- 25 April 2024, e13
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Associations between body weight change and incidence of major depressive disorder in patients with type 2 diabetes mellitus: a nationwide longitudinal follow-up cohort study of 1.1 million
-
- Journal:
- Psychological Medicine / Volume 54 / Issue 10 / July 2024
- Published online by Cambridge University Press:
- 12 March 2024, pp. 2380-2388
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Dysfunction of circulating endothelial progenitor cells in major depressive disorder
-
- Journal:
- Acta Neuropsychiatrica / Volume 36 / Issue 3 / June 2024
- Published online by Cambridge University Press:
- 05 January 2024, pp. 153-161
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Mental illness and cardiovascular health: observational and polygenic score analyses in a population-based cohort study
-
- Journal:
- Psychological Medicine / Volume 54 / Issue 5 / April 2024
- Published online by Cambridge University Press:
- 14 September 2023, pp. 931-939
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
ICD-11 and bipolar II disorder: so much ado and yet nothing new
-
- Journal:
- The British Journal of Psychiatry / Volume 223 / Issue 2 / August 2023
- Published online by Cambridge University Press:
- 01 August 2023, pp. 345-347
- Print publication:
- August 2023
-
- Article
-
- You have access
- HTML
- Export citation
School-based socio-emotional learning programs to prevent depression, anxiety and suicide among adolescents: a global cost-effectiveness analysis
-
- Journal:
- Epidemiology and Psychiatric Sciences / Volume 32 / 2023
- Published online by Cambridge University Press:
- 12 July 2023, e46
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Lurasidone and risk of metabolic syndrome: results from short and long-term studies in patients with bipolar depression
-
- Journal:
- CNS Spectrums / Volume 28 / Issue 6 / December 2023
- Published online by Cambridge University Press:
- 24 March 2023, pp. 680-687
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
The male–female suicide ratio in Denmark plateaus at 2.7: an opportunity for targeted intervention?
-
- Journal:
- Acta Neuropsychiatrica / Volume 35 / Issue 1 / February 2023
- Published online by Cambridge University Press:
- 05 January 2023, pp. 61-62
-
- Article
- Export citation
The role of pre-pandemic depression for changes in depression, anxiety, and loneliness during the COVID-19 pandemic: Results from a longitudinal probability sample of adults from Germany
-
- Journal:
- European Psychiatry / Volume 65 / Issue 1 / 2022
- Published online by Cambridge University Press:
- 03 November 2022, e76
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
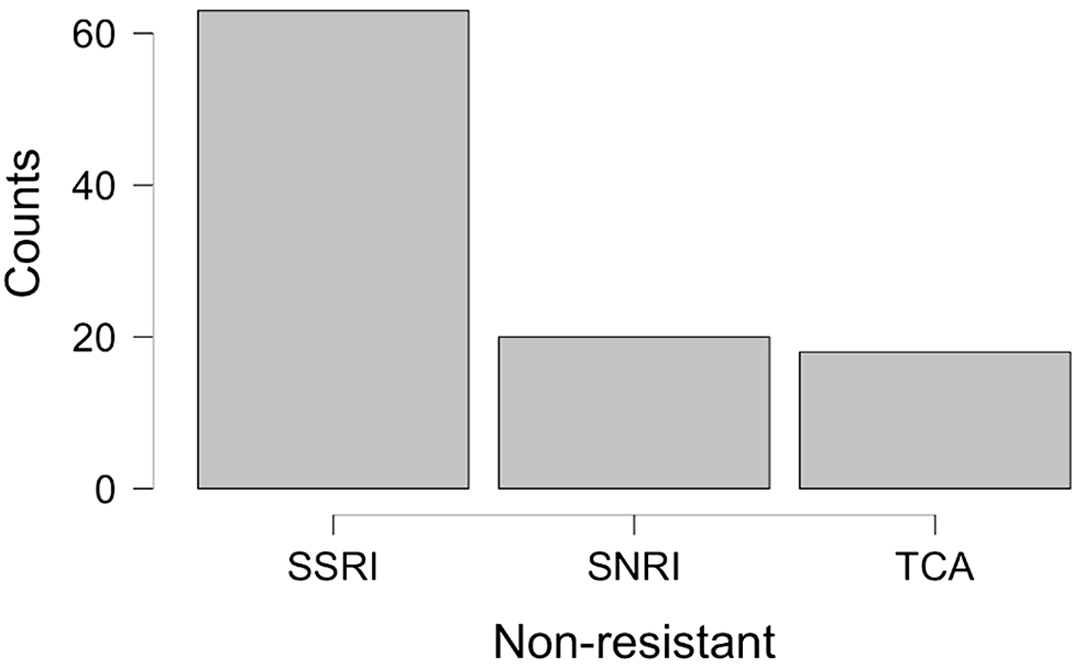
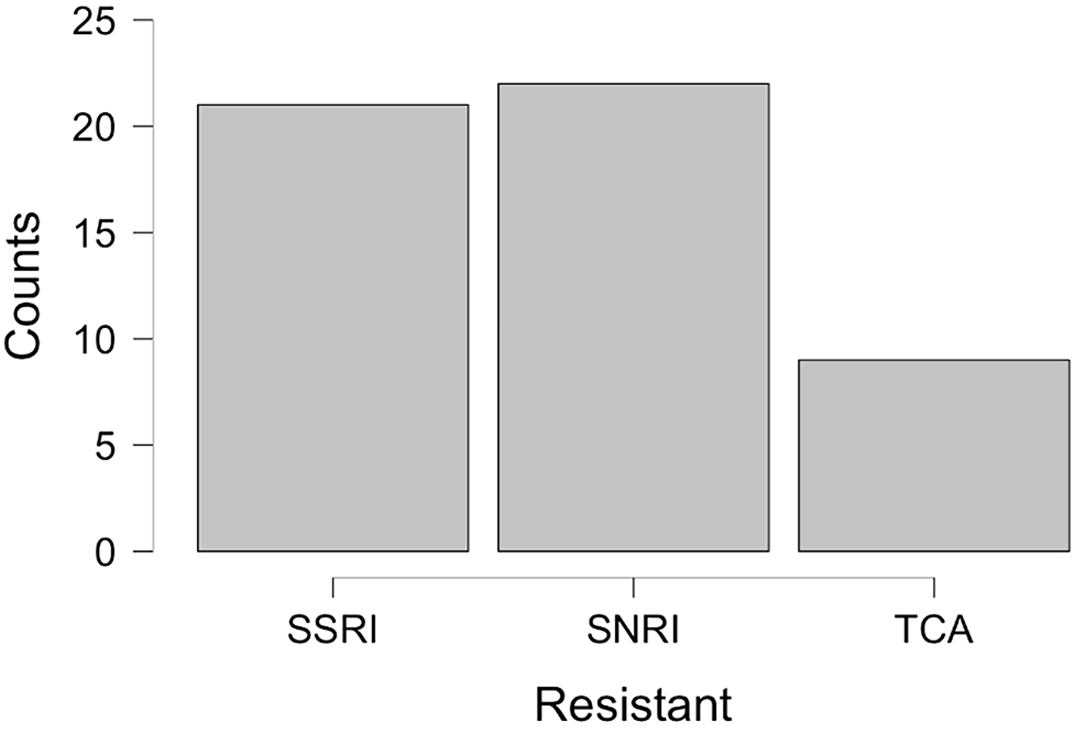
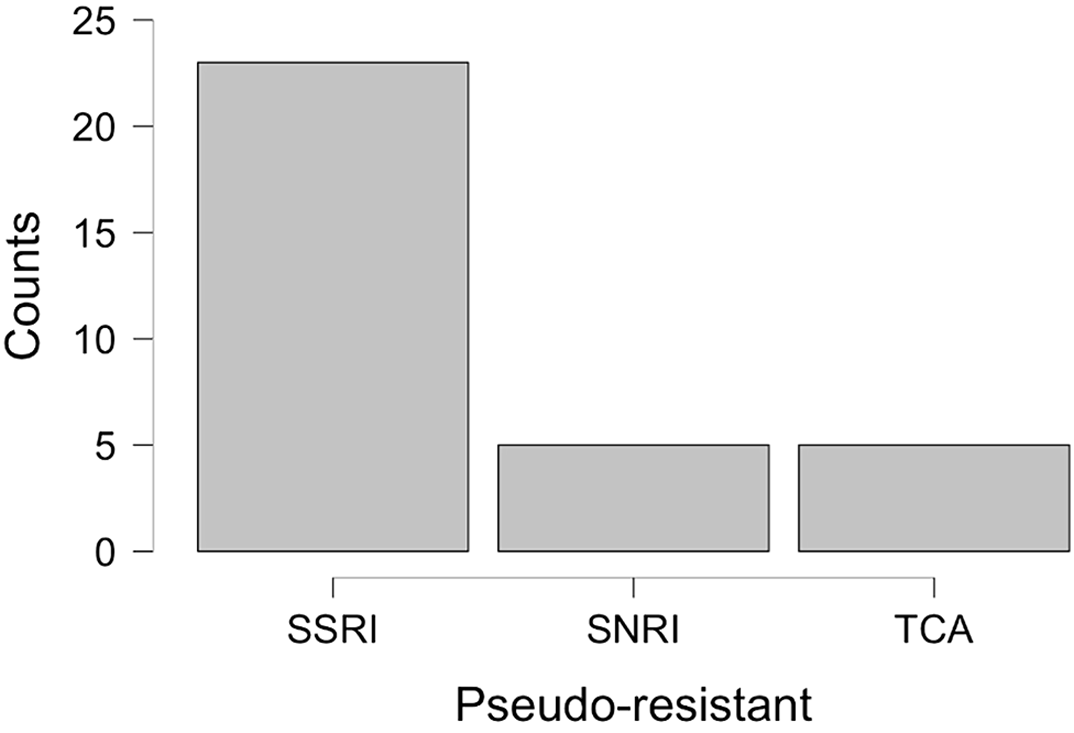
Resistance or pseudo-resistance?
-
- Journal:
- European Psychiatry / Volume 65 / Issue S1 / June 2022
- Published online by Cambridge University Press:
- 01 September 2022, pp. S370-S371
-
- Article
-
- You have access
- Open access
- Export citation
Association between Mood Disorders, Problematic Internet Use and Online Gambling Addiction: A Systematic Review
-
- Journal:
- European Psychiatry / Volume 65 / Issue S1 / June 2022
- Published online by Cambridge University Press:
- 01 September 2022, p. S834
-
- Article
-
- You have access
- Open access
- Export citation
comparisation of ABO blood groups between female patiens diagnosed with depressive disorders an bipolar affective disorders
-
- Journal:
- European Psychiatry / Volume 65 / Issue S1 / June 2022
- Published online by Cambridge University Press:
- 01 September 2022, p. S851
-
- Article
-
- You have access
- Open access
- Export citation
Attitudes towards death in adolescents hospitalized with depressive disorder
-
- Journal:
- European Psychiatry / Volume 65 / Issue S1 / June 2022
- Published online by Cambridge University Press:
- 01 September 2022, p. S560
-
- Article
-
- You have access
- Open access
- Export citation